What Are The Side Effects Of Treatment
Generally, the side effects of hormonal therapies tend to be mild and fairly well tolerated, says Brufsky. The most common side effects are menopausal symptoms , achiness in the joints and bones, and fatigue. AIs can cause some bone loss , but that can typically be well controlled with bone-modifying medications, Brufsky notes. CDK4/6 inhibitors may cause low white blood cell counts as well as some nausea and diarrhea.
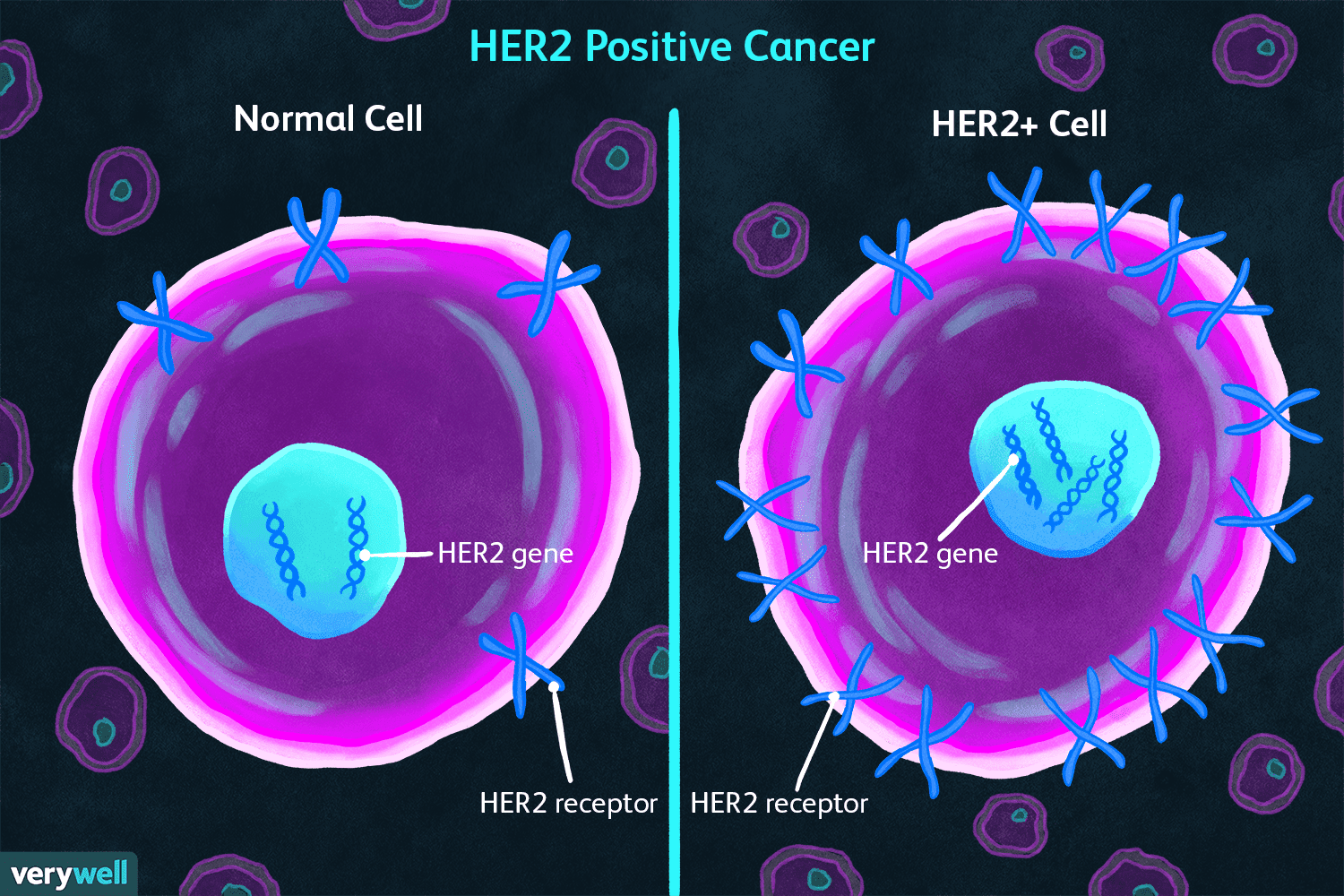
What Is Her2 And What Does It Mean
HER2 is a growth-promoting protein on the outside of all breast cells. Breast cancer cells with higher than normal levels of HER2 are called HER2-positive. These cancers tend to grow and spread faster than other breast cancers, but are much more likely to respond to treatment with drugs that target the HER2 protein.
Relevance Of The Oestrogen Receptor
Pathological complete response rates stratified by ER status and treatment arm in clinical trials of neoadjuvant HER2-targeted therapy for HER2+ breast cancer.
a | Pathological complete response rates observed with HER2-targeted therapy in combination with chemotherapy. b | pCR rates observed with HER2-targeted therapy, plus endocrine therapy for the oestrogen receptor-positive patient subgroups, without chemotherapy. For some trials, ER status actually reflects the hormone receptor status . L, lapatinib P, pertuzumab T, trastuzumab. aDocetaxel and carboplatin plus T + P. b5-fluorouracil, epirubicin and cyclophosphamide plus T + P followed by docetaxel plus T + P. c5-fluorouracil, epirubicin and cyclophosphamide followed by docetaxel plus T + P, dChemotherapy-free arm
Together, these data suggest that simultaneous inhibition of the HER2 and ER signalling pathways has the potential to be more effective than suppression of either pathway alone although the optimal treatment strategy for HER2+/HR+ breast cancer remains unclear, ER blockade seems to be necessary in patients with this disease subtype. Moreover, the optimal timing, sequencing and duration of ER inhibition, and how much chemotherapy is required with this strategy, remain open questions.
You May Like: Is Stage 3 Breast Cancer Curable
What Is My Her2 Status
HER2 is another type of growth signal receptor which may be present on your breast cancer cells. About 25% of breast cancers are HER2-positive. HER2-positive cancers are a mix of good and bad news.
The bad news is the tumors tend to grow more aggressively than those without the HER2 receptor. The good news is that like ER/PR-positive cancers, medicines can switch the HER2 growth receptor off.
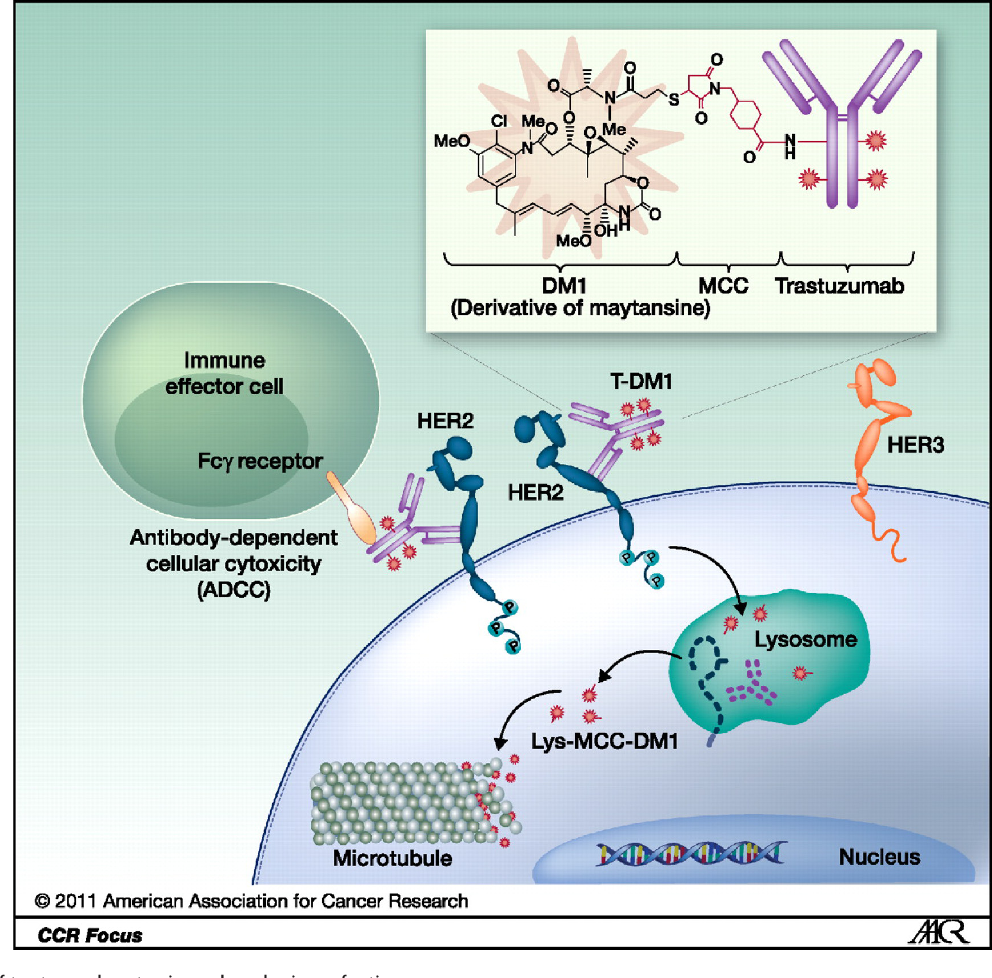
New drugs such as trastuzumab, pertuzumab, T-DM1 and lapatinib are extremely effective at this and have dramatically improved the prognosis for HER2-positive patients, Dr. Abraham says. Treatment outcomes are now as good as those with HER2-negative tumors.
But HER2-positive tumors bigger than half a centimeter or that have spread into the lymph nodes may require treatment with chemotherapy and one of the medicines specifically targeting the HER2 receptor, such as trastuzumab.
Conflict Of Interest Disclosures
Sonia Pernas reports personal fees and nonfinancial support from Roche, and other support from Polyphor, all outside the submitted work. Sara M. Tolaney reports institutional research funding from Novartis, Genentech, Eli Lilly, Pfizer, Merck, Exelixis, Eisai, Bristol Meyers Squibb, AstraZeneca, and Nektar and personal fees from Novartis, Eli Lilly, Pfizer, Merck, AstraZeneca, Eisai, Nektar, and Nanostring. Romualdo Barroso-Sousa made no disclosures.
Also Check: Is Breast Cancer Curable In The 3 Stage
Cish And Silver In Situ Hybridization
The CISH approach and SISH method capture the advantages of both IHC and FISH. It detects HER2 gene-copy number by using a single HER2 probe. The CISH was approved by the FDA to evaluate feasibility for anti-HER2 agent. In addition, CISH has the lowest correlation with IHC 2 staining and highest with IHC 0, 1, and 3 results. Previous researches have shown about 9799% of concordance between CISH and FISH. Several clinical trials have defined criteria as 3+ for IHC test or FISH-positive tumors whereas others, like the Finland Herceptin trial, have relied on the CISH results. However, this method needs further investigations in future.
Side Effects And Quality Of Life
Women treated with Herceptin and chemotherapy were more likely to have a severe side effect not related to blood counts compared to women treated with Herceptin alone 29.8% vs. 11.9%.
The most common side effects of any grade were:
- low white blood cell counts
- loss of appetite
- fatigue
- nausea
Health-related quality of life scores went down faster in women treated with Herceptin plus chemotherapy, compared to women treated with Herceptin alone, 2 months after starting treatment and 1 year after starting treatment.
In light of the lower toxicity and more favorable profile, trastuzumab monotherapy can be considered an adjuvant therapy option for selected older patients, the researchers wrote.
In an editorial accompanying the article, researchers not affiliated with the study agreed with the conclusion.
on the basis of the results of the RESPECT trial, it is possible to consider that adjuvant trastuzumab monotherapy could be an option for a subset of patients, particularly those who may have a higher risk of toxicity with chemotherapy and those with a lower anatomic risk of disease recurrence , they wrote. It is important to stress, however, that the choice of therapy in older patients should never be made on the basis of age alone. Comprehensive geriatric assessment is the standard of care for evaluation before chemotherapy and should generate a care plan to be implemented during treatment to minimize the risk of complications and maintain and functionality.
Read Also: What Are The Chances Of Getting Breast Cancer Twice
How Can Hormone Receptors Be Used To Slow Cancer Growth
Blocking the action of estrogen and/or progesterone could possibly stop the cancer from growing. There are a few ways in which this can happen:
- Blocking the hormone receptor with another compound prevents the estrogen or progesterone from being able to attach to the receptor and activate the cell.
- Prevent the body from making the hormone: This can be done with medication to block the production of the hormone, or with surgery to remove the organ that makes it. For example, estrogen production can be significantly decreased by surgically removing the ovaries.
- Eliminate the hormone receptors on cells or change their shape: This makes it impossible for the hormone to attach itself to the cell receptor and to activate it, essentially making the hormone unable to function.
What Is The Life Expectancy For Each Cancer Stage
Your outlook depends on the stage of your cancer when its discovered. Cancer is staged by number, starting with 0 and going to 4. Stage 0 is the very beginning and stage 4 is the last stage, also called the metastatic stage because its when cancer has spread to other areas in the body.
Each number reflects different characteristics of your breast cancer. These include the size of the tumor and whether cancer has moved into lymph nodes or distant organs, like the lungs, bones, or brain.
The cancer subtype doesnt play a role in staging, only in treatment decisions.
Survival statistics of women with the major subtypes of breast cancer such as ER-positive, HER2-positive, and triple-negative are grouped together. With treatment, most women with very early stage breast cancers of any subtype can expect a normal life span.
Survival rates are based on how many people are still alive years after they were first diagnosed. Five-year and 10-year survival are commonly reported.
According to the American Cancer Society, 5-year survival rates are:
- stage 0 100 percent
- stage 3 72 percent
- stage 4 22 percent
One thing to note is that these statistics also included women with the more aggressive HER2-positive and triple-negative cancers. And it takes five years to get to a five-year statistical survival rate, so newer therapies are not included in these numbers.
Its likely that a woman with ER-positive breast cancer diagnosed today may have a higher chance of survival.
Also Check: Is Breast Cancer Curable In The 3 Stage
Breast Cancer Hormone Receptor Status
Breast cancer cells taken out during a biopsy or surgery will be tested to see if they have certain proteins that are estrogen or progesterone receptors. When the hormones estrogen and progesterone attach to these receptors, they fuel the cancer growth. Cancers are called hormone receptor-positive or hormone receptor-negative based on whether or not they have these receptors . Knowing the hormone receptor status is important in deciding treatment options. Ask your doctor about your hormone receptor status and what it means for you.
You May Like: Can You Be An Organ Donor After Breast Cancer
Testing For Her2 Status
There are several tests used to find out if breast cancer is HER2-positive. How your results appear in the report will depend on the test you have. Two of the most common tests are:
- IHC test : The IHC test uses a chemical dye to stain the HER2 proteins. The IHC gives a score of 0 to 3+ that measures the amount of HER2 proteins on the surface of cells in a breast cancer tissue sample. If the score is 0 to 1+, its considered HER2-negative. If the score is 2+, it’s considered borderline. A score of 3+ is considered HER2-positive. If the IHC test results are borderline, its likely that a FISH test will be done on a sample of the cancer tissue to determine if the cancer is HER2-positive.
- FISH test : The FISH test uses special labels that attach to the HER2 proteins. The special labels have chemicals added to them so they change color and glow in the dark when they attach to the HER2 proteins. This test is the most accurate, but it is more expensive and takes longer to return results. This is why an IHC test is usually the first test done to see if a cancer is HER2-positive. With the FISH test, you get a score of either positive or negative .
It’s important to know which HER2 test you had. Generally, only cancers that test IHC 3+ or FISH positive respond to the medicines that target HER2-positive breast cancers. An IHC 2+ test result is called borderline. If you have an IHC 2+ result, ask to have the tissue retested with the FISH test.
You May Like: What Is Stage 3a Breast Cancer
How Her2 Affects Treatment
Treatment for breast cancer depends in part on the stage and type and is different in each case, but typically involves some combination of surgery, radiation, chemotherapy, or other drug therapies. These other drug therapies depend partly on whether your cancer is HER2-positive. If it is, certain medications can work well, such as:
Monoclonal antibodies. These are lab-made versions of immune system substances designed to attach to HER2 protein on breast cancer cells.
Antibody-drug conjugates. These drugs target chemotherapy directly to HER2 protein on cancer cells.
Kinase inhibitors. These medications stop proteins like HER2 from sending signals.
Donât Miss: What To Say To Someone Diagnosed With Breast Cancer
Evolving Thoughts On Surgery
When breast cancer is metastatic at the time of diagnosis, surgery has not usually been done, as it was believed that it didn’t improve survival rates. This thought appears to be changing, with evidence that primary surgery in people with stage 4 HER2-positive breast cancer improves overall survival. In addition, when a breast tumor is causing symptoms , palliative mastectomy may significantly reduce symptoms. In a 2018 study, palliative mastectomy was found to improve quality of life for some people.
You May Like: How To Cure Breast Cancer With Baking Soda
Mrna Evaluation By Microarray And Reverse Transcription Polymerase Chain Reaction
In breast cancer management, microarray-based mRNA measurements can assess relative levels of different mRNA molecules. Several multigene predictor assays, including Oncotype DX, Mammaprint, and TargetPrint, have been approved. These assays utilize HER2 mRNA associated with other genes related to HER2 amplification, in evaluating recurrence risk of breast cancer.
Relative levels of HER2 mRNA can also be detected by RT-PCR technique, although large-scale trials have not yet been conducted. This approach is relatively rapid, low cost, and has tremendous potential. Enzyme-linked immunosorbent assay can be used to detect the concentration of protein in extracellular domain of tissue and serum. This technique has been approved by the FDA in the monitoring of disease, using commercially available kit like Oncogene Science HER2/neu ELISA . Recently, a meta-analysis purposed that assessment of HER2 ECD levels in breast cancer may not be informative. Moreover, collective analysis of four trials showed that the baseline ECD level was not reliably predictive of response to the therapy. Contrarily, some studies have shown supporting data of the relationship between ECD levels and response to specific therapies. Thus, further investigation needs to be done to arrive at conclusion about the utility of HER2 ECD assessment.
N Categories For Breast Cancer
N followed by a number from 0 to 3 indicates whether the cancer has spread to lymph nodes near the breast and, if so, how many lymph nodes are involved.
Lymph node staging for breast cancer is based on how the nodes look under the microscope, and has changed as technology has improved. Newer methods have made it possible to find smaller and smaller collections of cancer cells, but experts haven’t been sure how much these tiny deposits of cancer cells affect outlook.
Its not yet clear how much cancer in the lymph node is needed to see a change in outlook or treatment. This is still being studied, but for now, a deposit of cancer cells must contain at least 200 cells or be at least 0.2 mm across for it to change the N stage. An area of cancer spread that is smaller than 0.2 mm doesn’t change the stage, but is recorded with abbreviations that indicate the type of special test used to find the spread.
If the area of cancer spread is at least 0.2 mm , but still not larger than 2 mm, it is called a micrometastasis . Micrometastases are counted only if there aren’t any larger areas of cancer spread. Areas of cancer spread larger than 2 mm are known to affect outlook and do change the N stage. These larger areas are sometimes called macrometastases, but are more often just called metastases.
NX: Nearby lymph nodes cannot be assessed .
N0: Cancer has not spread to nearby lymph nodes.
N1c: Both N1a and N1b apply.
N3: Any of the following:
N3a: either:
N3b: either:
Don’t Miss: Can Asbestos Cause Breast Cancer
Neratinib In Cns Disease
The phase II NEfERT study directly compared neratinib against trastuzumab in combination with paclitaxel in the first-line setting for HER2+ MBC. Although the neratinib arm was not superior to trastuzumab in terms of overall PFS, it did reduce the risk of CNS recurrence by 50%, from 17.3% in the trastuzumab arm to 8.3% in the neratinib arm .74 The risk of CNS progression was also lower in the neratinib arm .74 Neratinibs apparent ability to control CNS disease was consistently observed across patients with and without baseline brain metastases. As previously, the neratinib/paclitaxel arm was associated with a 30% risk of G3-4 toxicities , predominantly G3 diarrhoea.74
Although only patients with treated, stable brain metastases were included in the NALA study, notably fewer patients treated with neratinib required CNS intervention , further confirming its superior CNS activity compared to lapatinib.70
Unfortunately, the adjuvant phase III ExteNET study where a year of adjuvant neratinib following 12 months of trastuzumab was found to significantly prolong IDFS, neratinib did not significantly reduce the incidence of CNS recurrence over 5 years in comparison to placebo, although the number of events was very low in both arms , so it is difficult to draw any meaningful conclusions.76
Read Also: Can Metastatic Breast Cancer Go Into Remission
Types Of Breast Cancer
There are different types of breast cancer. Knowing the type of breast cancer you have helps your doctors decide on the best treatment for you.
On this page
There are different types of breast cancer. Knowing the type of breast cancer you have helps your doctor to plan the best treatment for you.
Breast cancer can be non-invasive or invasive.
Non-invasive breast cancer stays within the ducts or lobules and is called ductal carcinoma in situ .
Invasive breast cancer is when the cancer cells spread outside the milk ducts or lobules where they first started. Most breast cancers are invasive and can be grouped as:
- no special type
Other less common types of invasive breast cancer include:
- invasive lobular breast cancer
- inflammatory breast cancer
- Pagets disease of the breast.
Some breast cancers are also identified by whether or not the cancer cells have receptors for hormones or a protein called HER2 .
Breast cancer that does not have receptors for HER2 or hormones is called triple negative breast cancer.
This is the earliest form of breast cancer. In DCIS there are cancer cells in the ducts of the breast but these cells are contained . They have not spread into normal breast tissue.
DCIS may show up on a mammogram and is commonly diagnosed when women have breast screening.
Invasive breast cancer means the cancer cells have spread outside the lining of the ducts or lobes and into the surrounding breast tissue. There are different types of invasive breast cancer.
You May Like: Harrington Breast Cancer Center Amarillo Tx
What Is The Grade Of My Tumor
Grading is not the same as staging. Both are indicators of a cancers severity and prognosis, but they use different criteria. Staging deals with the tumor size, location and the distribution of cancer cells in your body. But grading is based on how the cancer cells appear under a microscope.
The more abnormal-looking the cells are, the more likely they are to quickly grow and spread. Grades usually run from I to III. A higher grade is a more aggressive cancer. Its possible to have a Stage I tumor thats also a Grade III cancer.
Will I Need Radiation
Most oncologists generally recommend radiation treatment for all breast cancer patients who undergo only removal of the tumor .
For women who undergo whole-breast removal, radiation may be recommended for those who are considered high-risk, especially those with tumors larger than 5 centimeters and with more than four cancerous lymph nodes.
You May Like: Did Anne Hathaway Have Breast Cancer