What Is The Factor That Leads To Her2 Positive Breast Cancer
Scientists still cannot answer the question of what causes HER2 positive breast cancer. However, according to the ongoing research conducted by scientists, genetic factors, lifestyle and the environment are thought to have effects on HER2 positivity. It is thought that the risk of HER2 positivity increases in the following situations:
- Women
- Obesity
- Family history of breast cancer
- Giving birth after the age of 30
- Previous radiation therapy
- Smoking
As far as the ongoing studies show, approximately 25% of all breast cancer patients are HER2 positive. High levels of HER2 protein are encountered due to overexpression caused by a mutation in the HER2 gene. HER2 produced at high levels causes uncontrolled proliferation of cells.
What Do The Test Results Mean
The results of HER2 testing will guide you and your cancer care team in making the best treatment decisions.
It is not clear if one test is more accurate than the other, but FISH is more expensive and takes longer to get the results. Often the IHC test is done first.
- If the IHC result is 0 or 1+, the cancer is considered HER2-negative. These cancers do not respond to treatment with drugs that target HER2.
- If the IHC result is 3+, the cancer is HER2-positive. These cancers are usually treated with drugs that target HER2.
- If the IHC result is 2+, the HER2 status of the tumor is not clear and is called “equivocal.” This means that the HER2 status needs to be tested with FISH to clarify the result.
Triple-negative breast tumors dont have too much HER2 and also dont have estrogen or progesterone receptors. They are HER2-, ER-, and PR-negative. Hormone therapy and drugs that target HER2 are not helpful in treating these cancers. See Triple-negative Breast Cancer to learn more.
Triple-positive breast tumorsare HER2-, ER-, and PR-positive. These cancers are treated with hormone drugs as well as drugs that target HER2.
Our team is made up of doctors and oncology certified nurses with deep knowledge of cancer care as well as journalists, editors, and translators with extensive experience in medical writing.
Last Revised: September 20, 2019
A Number Of Clinical Studies Provided Evidence
Since the development and usage of trastuzumab, the international field of breast cancer study has carried out a number of large scale classic adjuvant therapy in clinical studies, including NSABP B-31, NCCTG9831, HERA, FinHer and BCIRG006, etc. , all having explored the efficacy, the treatment time and the best treatment modality using trastuzumab in HER2-positive breast cancer patients. The results of these studies have subsequently confirmed that the adoption of trastuzumab for HER2-positive breast cancer can reduce the risk of recurrence of early breast cancer by about 50% and lower the risk of death by about 30%.
N9831 and NSABP B-31 studies have compared the adjuvant treatment efficacy in HER2-positive breast cancer patients with AC-T program with or without trastuzumab, jointly analysing the patient overall survival and disease-free survival . The results showed that the DFS rate of patients with trastuzumab had significantly improved over the group of patients without trastuzumab treatment , the OS rate was also significantly increased . The cumulative incidences of distant metastasis in the trastuzumab usage group had an absolute reduction of 9.6%.
Recommended Reading: Chances Of Getting Breast Cancer Twice
Do Symptoms And Signs Of Her2
The signs and symptoms for HER2-positive breast cancers are the same as for HER2-negative breast cancers, except for the fact that HER2-positive cancers are likely to grow faster and are more likely to spread. The following are possible signs of breast cancer:
- Thickening or lump in the breast that feels different from the surrounding area
- Inverting of the nipple
What Is Metaplastic Carcinoma

Also known as metaplastic breast cancer, metaplastic carcinoma is a rare type of invasive breast cancer with a unique characteristic: It contains a mix of two or more types of breast cancer cells, usually carcinoma combined with sarcoma. Metaplastic means that one form is turning into another. Various leading-edge techniques are used to analyze the exact genetics and biology of these confused cancers to find out if the tumor is more similar to carcinoma or sarcoma, since these two types of cancer have very different treatments.
Also Check: Is Breast Cancer Curable In The 3 Stage
Tests For Brca And Other Gene Mutations
A genetic test can tell you if you have any mutations in genes that are related to an increased risk of breast cancer. Its important to know that genetic testing is most helpful when you have a strong family history of either breast or ovarian cancer or a personal history of breast cancer.
If youd like to be tested, contact your doctor or your hospitals education office. Ask for a recommendation for a genetic counselor. Make an appointment and discuss the risks of undergoing genetic testing.
Your genes may affect your risk for breast cancer, but your lifestyle can have an impact as well. Whether or not you have a genetic mutation, its important to lower your risk whenever you can.
The following preventive measures may help you avoid a breast cancer diagnosis.
Her2 Regulates Mammary Stem/progenitor Cell Populations
All tissues in the body are derived from organ-specific stem cells that have the capacity to undergo self-renewal, differentiate into the cell types that comprise each organ, and help maintain tissue integrity. There is some evidence that certain tumors are derived from stem cells or from early descendents of stem cells. Bonnet et al discovered that leukemia is driven by a small population of leukemia cells that have the ability to perpetually self-renew. They termed this population cancer stem cells .
In contrast to the traditional stochastic model of oncogenesis where transformation results from random mutations and subsequent clonal selection, the CSC model postulates that cancer originates in tissue stem cells through dysregulation of self-renewal pathways . As a result, tumors contain and are driven by a subpopulation of cells that retains key stem-cell properties including self-renewal, which drives tumorigenesis, and differentiation, which contributes to cellular heterogeneity. This leads to expansion of this cell population that may undergo subsequent genetic and epigenetic changes, and the only cells within an organism that live long enough to accumulate the necessary mutations that lead to cancer are stem cells.
Read Also: Why Is Left Breast Cancer More Common
Her2 Promotes Early Dissemination Of Incompletely Transformed Cells
Metastasis, the primary cause of morbidity and mortality of most cancers, is an extremely complex and highly organized process that is organ specific and involves numerous reciprocal interactions between the cancer cells and the host . The stage at which individual cells leave the primary tumor was unclear, and new data have caused us to rethink this process. The previous metastasis model suggested that epithelial cells sequentially accumulate multiple genetic and epigenetic changes underlying the disorganization of tissue morphology and uncontrolled growth . The model predicted that certain additional genomic events initiate invasiveness of the tumor and metastasis in the final stages of tumorigenesis.
In contrast, in situ carcinomas already display chromosomal aberrations very similar to invasive carcinomas . Likewise, similar genetic alterations were observed in primary tumors and synchronous regional lymph node metastasis . In contrast, asynchronous distant metastases often differ extensively from the corresponding matched primary tumors . Early disseminated cancer cells are genomically very unstable, and selection of clonally expanding cells leading to metastasis seems to occur after dissemination has taken place . Overall, the data indicates that the molecular heterogeneity that characterizes invasive breast cancers occurs at the time of initial progression .
Will I Need To Do Anything To Prepare For The Test
You won’t need any special preparations if you are getting local anesthesia . If you are getting general anesthesia, you will probably need to fast for several hours before surgery. Your surgeon will give you more specific instructions. Also, if you are getting a sedative or general anesthesia, be sure to arrange for someone to drive you home. You may be groggy and confused after you wake up from the procedure.
Recommended Reading: Anne Hathaway Breast Implants
Why Receptor Status Matters
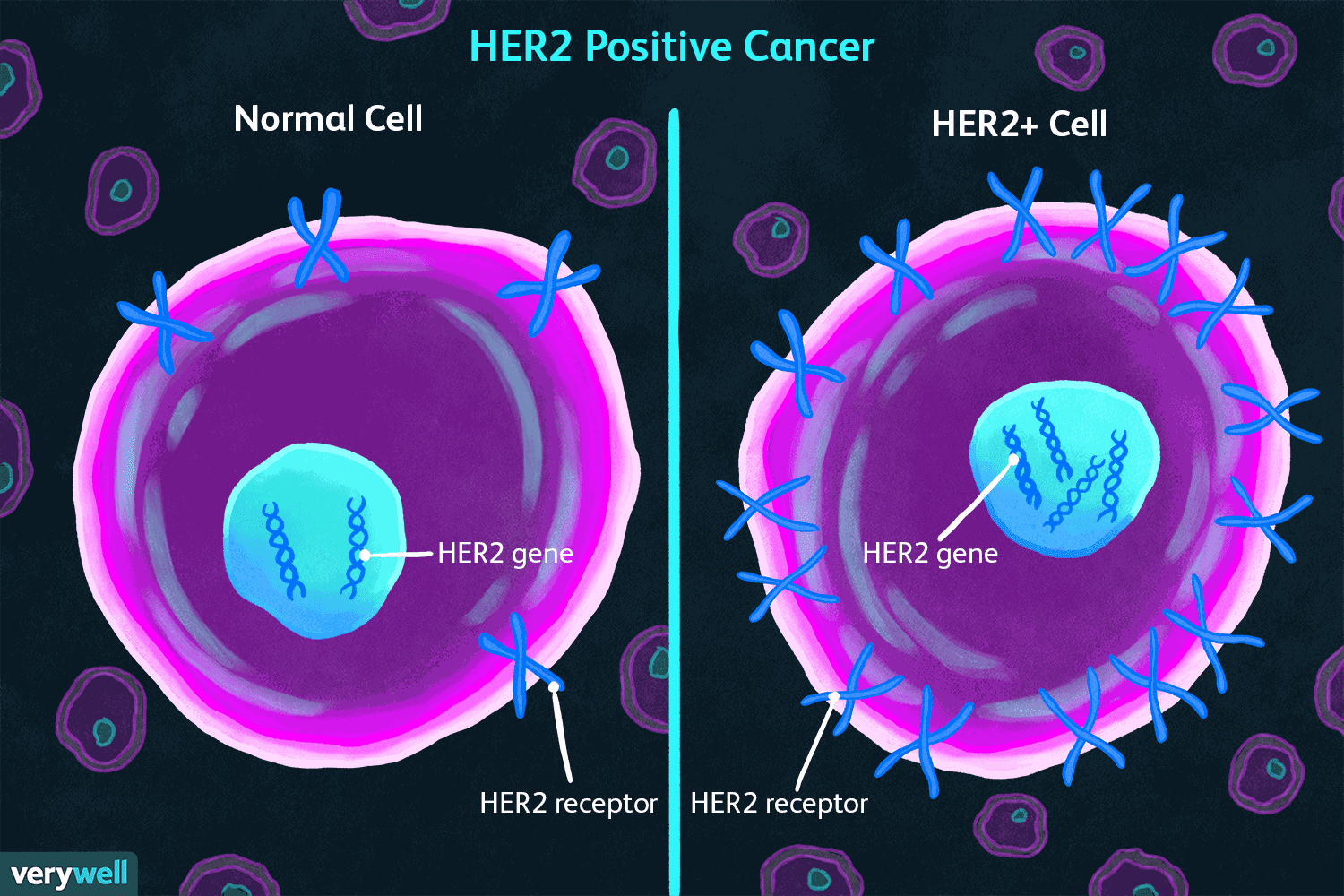
Breast cancer is not a single disease, and researchers now have the ability to break down breast cancer into different subtypes based on the receptor status of the tumors. Among the variations between different types of breast cancers are the proteins found on cell surfaces, which are involved tumor growth. These proteins are related to the genetic material of cancer cells.
For example, with estrogen receptor-positive breast cancer, estrogen binds to specific receptors on breast cancer cells, stimulating proliferation. Similarly, HER2 receptors on the surface of breast cancer cells are stimulated by HER2 protein, promoting the growth and spread of breast cancer.
It’s important to note, however, that all breast cellsboth cancerous and noncanceroushave HER2 receptors other their surfaces. The difference is that HER2-positive breast cancer cells have 40 to 100 times more receptors than HER2-negative breast cancer cells or normal breast cells. In positive cases, the abundance of receptors fuels the cancer.
Breast Cancer Discussion Guide
Get our printable guide for your next healthcare provider’s appointment to help you ask the right questions.
Molecular And Genomic Classification Of Breast Cancer
Expression analysis has provided an opportunity to explore comprehensive molecular profiling of BC. Differences in gene expressions patterns display basic alterations in the tumor cell biology and are associated with significant variation in terms of clinical behavior, survival , and treatment outcomes . The identification of several molecular subtypes was the first insight into the molecular heterogeneity of the BC . Five main intrinsic subtypes have been identified based solely on gene expression patterns using DNA microarrays : luminal A, luminal B, HER2 overexpressing or HER2-enriched and basal like, with another less characterized group named normal breast-like. They are called as intrinsic subtypes of breast cancer and they have exposed crucial differences in several aspects. The tumor heterogeneity within hormone receptor-positive breast cancers are encompassed by the luminal A and luminal B subtypes, with better survival outcomes with respect to the non-luminal intrinsic subtypes. The luminal B breast tumor expresses hormonal receptors same as the luminal A subtype, but generally having low PR, high proliferation, high grade and worse response to hormonal therapy. At the molecular level, this subtype seems to be dramatically distinct from luminal A, at levels of gene expression, gene copy, or somatic aberrations. All of these features, confers it worse prognosis than the other luminal intrinsic subtype .
Don’t Miss: How To Cure Breast Cancer With Baking Soda
Her2 Positive Breast Cancer Recurrence
HER2 positive breast cancer is an aggressive disease with an elevated risk of metastatic spread if appropriate treatment or therapy is not administered. While HER2 positive breast cancer recurrence affects some patients, recent advancements in targeted therapies and long-term treatment approaches have made relapse less likely than ever before. The majority of patients with HER2 positive cancer do not experience recurrence.
Despite these odds, you may still feel nervous about your chances of cancer recurrence if you have a history of HER2 positive breast cancer. This is completely understandable. The best way to calm your fears and reduce your risk is to be proactive about your breast health, complete all recommended treatments or therapies, and maintain regular follow-up with your breast cancer clinical care team.
Actin Fiber Staining And Confocal Microscopy
Tzm-resistant SKBR3 cells were seeded and incubated on Matrigel-coated 4-well chamber slides in complete EBM-2 medium for 30min. Then, the medium was replaced with Hanks balanced salt solution supplemented with 0 or 4M salinomycin, and the cells were further incubated for 2h. The cells were fixed with 4% paraformaldehyde for 10min at room temperature. After permeabilization with 0.2% Triton X-100 for 2min, filamentous actin was stained with ActinGreen 488 Ready Probe for 30min. Nuclei were counterstained with DAPI, and confocal images were obtained using an FV10i confocal laser scanning microscope . The amount of F-actin in a cell was quantified using ImageJ software and was represented as integrated density.
Read Also: How To Donate To Breast Cancer Charity
Taking Care Of Yourself
Having breast cancer can be overwhelming. Remember, though: You’re in control of your treatment decisions and how you live your life.
These tips can help you stay healthy while you get treatment:
- Get the support you need. This could be information about breast cancer, talking with someone, or help with daily tasks. It can all make a huge difference in how you feel. Listen to your body. Exercise can help you feel better, but only when you’re up for it.
- Stay nourished. If you don’t have much of an appetite, eat smaller meals every few hours rather than three big meals.
What Tests Detect Her2
All patients with invasive breast cancer should have their tumor cells tested for HER2. Medical professionals routinely perform this test in the pathology laboratory at the time of diagnosis, using the sample of your breast tissue removed for diagnosis. The testing for HER2 can involve one or more of the following tests.
Health care professionals may use either immunohistochemistry to identify the HER2 protein or in-situ hybridization testing to look for the gene.
Don’t Miss: Did Anne Hathaway Have Breast Cancer
It’s A Hopeful Time For Her2
If you or a loved one are diagnosed with this cancer, remember this: There are more effective treatments available than ever. The big take-home point about HER2-positive tumors is that while this is very aggressive tumor, these very targeted treatments are incredibly effective, Dr. Kulkarni says. So while prognosis used to be poor, with the introduction of targeted treatments and more to come, people see much better outcomes, she says. Its very exciting times for HER2-positive breast cancer research, Dr. Czerniecki says.
The Details: In Depth Analysis Of The Impact Of Anti
Research data set forth above has illustrated the current status of anti-HER2 therapy in China and in the USA. Will the adoption of targeted therapy for HER2-positive breast cancer affect the survival of patients, and if so, how much is the impact? We will look for answers through clinical data and analysis on real-world treatment conditions.
You May Like: What Does Triple Negative Mean For Breast Cancer
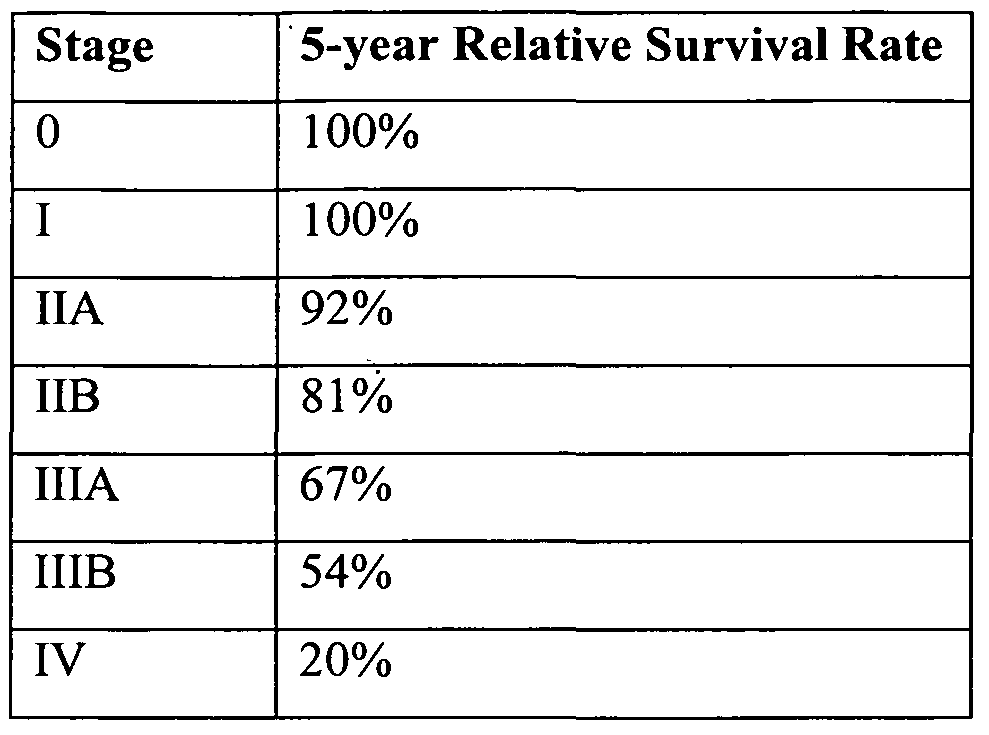
Risk Of Recurrence: Early And Late
Research has shown the HER2-positive early breast cancers are two to five times more likely to recur than HER2-negative tumors. Even very small HER2-positive tumors with negative lymph nodes have a much higher risk of recurrence relative to tumors that are HER2-negative. Treatment with Herceptin can cut this risk by half.
The pattern of breast cancer recurrence may also differ. Small tumors are also more likely to have a metastatic recurrence if they are HER2-positive.
Despite the fact that HER2-positive and estrogen receptor-negative tuors are more likely to recur early on than estrogen receptor-positive and HER2-negative cancers, late recurrences are much less common.
With estrogen receptor positive breast cancers, the cancer is more likely to recur after 5 years than in the first 5 years, and the risk of recurrence remains steady each year for at least 20 years following the diagnosis. In contrast, those who have HER2 positive tumors and reach their 5 year mark are much more likely to be “in the clear” and remain recurrence free.
Side Effects Of Herceptin
Herceptin often causes side effects, although many of these will become less severe over time.
The following side effects are experienced by around 1 in 10 people:
- a reaction to the medicine, such as chills, a high temperature, swelling of the face and lips, headache, hot flushes, feeling sick, wheezing and breathlessness
- tiredness and difficulty sleeping
Cancer Research UK also has more information about the common side effects of herceptin.
Tell your doctor if you have particularly troublesome side effects, as there may be medicines available to treat them.
You May Like: How To Cure Breast Cancer With Baking Soda
Foods To Be Included In The Diets Of Her2 Positive Individuals
No diet has the power to prevent or cure cancer. However, a balanced and healthy diet is one of the necessary elements for the smooth progress of the process. The following foods are recommended to be consumed during the treatment.
- Citrus fruits are foods rich in flavonoid antioxidants. Flavonoid antioxidant is thought to have inhibitory effects on HER2 positive cancer growth.
- Black pepper contains an active compound called piperine, which is also a compound thought to be effective in slowing HER2 positive cancer growth.
- Omega-3 fatty acids regulate cholesterol levels and play a role in the treatment of diseases such as HER2 positive breast cancer.
Mechanisms Of Resistance To Her2
Intrinsic and acquired mechanisms of resistance to HER2-targeted agents have been described. HER2 reactivation or signaling downstream from the HER2 receptor are some of the commonly described mechanisms of resistance. HER2 mutations are a well-known intrinsic and acquired mechanisms of resistance,. Different types of mutations have been described, including activating mutations and mutations that modify the receptor preventing binding of monoclonal antibodies,,. L755S is the most frequently identified acquired activating mutation of HER2 which is more commonly seen in metastatic tumors. L755S has been described as an acquired mechanism of resistance to lapatinib and cross resistance to tucatinib has been reported in vitro. However, the resistant cells appear to be sensitive to neratinib, which is a pan-HER2 TKI,. More studies are needed to determine the clinical significance of this mutations to allow us to tailor treatment based on the specific mutations.
Also Check: Baking Soda And Honey For Cancer