Hereditary Breastovarian Cancer Syndrome
| Hereditary breastovarian cancer syndrome |
|---|
| Other names |
| Obstetrics and gynaecology, endocrinology, dermatology, oncology, medical genetics |
Hereditary breastovarian cancer syndromes are cancer syndromes that produce higher than normal levels of breast cancer, ovarian cancer and additional cancers in genetically related families . It accounts for 90% of the hereditary cancers. The hereditary factors may be proven or suspected to cause the pattern of breast and ovarian cancer occurrences in the family. The name HBOC may be misleading because it implies that this genetic susceptibility to cancer is mainly in women. In reality, both sexes have the same rates of gene mutations and HBOC can predispose to other cancers including prostate cancer and pancreatic cancer. For this reason, the term “King syndrome” has recently come into use. The new name references who identified the genes BRCA1 and BRCA2.
Related Genetic Counseling Issues
See Management, for information on evaluating at-risk relatives for the purpose of early diagnosis and treatment.
Family planning
- The optimal time for the determination of genetic risk and discussion of the availability of prenatal/ is before pregnancy.
- It is appropriate to offer to young adults who are affected or at risk.
Genetic cancer risk assessment and counseling. For a comprehensive description of the medical, psychosocial, and ethical ramifications of identifying at-risk individuals through cancer risk assessment with or without , see Cancer Genetics Risk Assessment and Counseling â for health professionals .
At-risk asymptomatic adult relatives. In general, relatives of an individual who has a BRCA1 or BRCA2 should be counseled regarding their risk of having inherited the same variant, their options for , their cancer risk, and recommendations for cancer screening and prophylactic surgery .
At-risk adult relatives who have not inherited the cancer-predisposing identified in the are presumed to be at or above the general population risk of developing cancer, depending on personal risk factors. For example, a female at-risk relative who does not have the family-specific BRCA1 or BRCA2 may still be at an elevated risk for breast cancer based on a breast biopsy history that revealed atypical ductal hyperplasia.
Surgery To Remove The Ovaries And Fallopian Tubes
- Surgery to remove the ovaries and fallopian tubes reduces the risk of:
- cancer of the ovaries and fallopian tubes by up to 95%
- breast cancer by 50% if done before the menopause
Surgery to remove these organs is only done when you have finished having a family. It is not possible to have children after this surgery.
The timing of surgery differs depending on the type of gene fault in your family and also on your own personal and family history.
- In families that carry a BRCA1 gene fault, cancer of the ovaries and fallopian tubes usually develops after the age of 40. Surgery is therefore recommended after the age of 35 and by the age of 40.
- In families that carry a BRCA2 gene fault, cancer of the ovaries and fallopian tubes usually develops at a later age.
Surgery is therefore recommended after the age of 40 and by the age of 45, but can be considered earlier.
Surgery to remove the ovaries and fallopian tubes can often be done by laparoscopic surgery which allows the operation to be done through a few tiny cuts in the tummy. The recovery from this surgery is usually quick, taking less than a week.
If you have had previous abdominal surgery or if you choose to have a hysterectomy at the same time, the operation may be done through a larger cut in the bikini line area.
A hysterectomy can sometimes be done through keyhole surgery depending on the size of the uterus and whether or not you have had previous surgery.
Read Also: What Are The Chances Of Her2 Positive Breast Cancer Returning
Breast Reconstruction Using Your Natural Body Tissue
Breast reconstruction can also be done using tissue from another part of the body to create a breast. This is usually done with tissue from:
- the lower tummy , called a transverse rectus abdominis myocutaneous flap, or deep inferior epigastric artery perforator flap or
- the back and shoulder blade area, called a latissimus dorsi flap, with or without an implant.
Breast reconstruction using natural body tissue is a much bigger operation than breast reconstruction using an implant. It takes many hours to perform. The recovery time is longer because there are other wounds that need to heal .
There are lots of things that may influence your choice of breast reconstruction.
Your body shape, your level of physical activity, your general fitness and personal preference are all things to be considered. The costs of all types of breast reconstruction may be covered by Medicare and also by private health funds.
If you are thinking about breast reconstruction, your doctor can refer you to a plastic surgeon experienced in breast reconstruction to discuss your options in detail.
What Is Hereditary Breast And Ovarian Cancer Syndrome
Some red flags in a patients medical record or family history may indicate a genetic tendency to develop ovarian cancer, including:
- A diagnosis of breast cancer at age 50 or earlier
- Bilateral breast cancers, either in you or in a close relative
- A close blood relation diagnosed with ovarian cancer
- Father, brother, uncle or grandfather with male breast cancer
- Triple-negative breast cancer diagnosed at age 60 or younger
- Ashkenazi Jewish ancestry
- A previously identified BRCA mutation in the family
If any of these apply to you, you may want to talk to your doctor about genetic testing and counseling.
Don’t Miss: What Are The Warning Signs Of Metastatic Breast Cancer
Screening For Ovarian Cancer
So far in the UK, screening is not offered for ovarian cancer. Current screening tests cannot find ovarian cancer early enough to make it more treatable. Researchers are still trying to find the most effective way to screen for ovarian cancer. Some women are offered screening as part of a clinical trial. Your doctor can explain if this is available and the possible risks and benefits of taking part in a clinical trial.
Genetic Testing And Ovarian Cancer
Just 3 percent of people with breast cancer have inherited mutations in BRCA genes. This means that most people diagnosed with breast cancer dont have a gene change that puts them at risk for ovarian cancer. However, you may be more likely to have one of these inherited mutations if you were diagnosed with breast cancer before the age of 50, developed breast cancer in both breasts, or have multiple family members including male family members who were diagnosed with breast cancer.
If your doctor thinks you may have a genetic mutation that leads to a higher risk of cancer, they may recommend genetic counseling and genetic testing. In this case, you will meet with a genetic counselor to talk about your cancer risk, and you may undergo tests that help determine whether you have certain gene changes. These tests are very simple and involve either a blood or saliva test. When one person within a family finds out they have an inherited gene change, other family members should be informed and may also want to be tested to determine their risk levels.
Also Check: Can Ovarian Cancer Cause Breast Pain
Does Your Family Health History Put You At Risk
Collect your family health history of breast, ovarian, and other cancers and share this information with your doctor. You can inherit BRCA and other mutations from your mother or your father, so be sure to include information from both sides of your family. Include your close relatives: parents, sisters, brothers, children, grandparents, aunts, uncles, nieces, nephews, and grandchildren. If you have had breast, ovarian, or other cancers, make sure that your family members know about your diagnosis.
Tell your doctor if you have a personal or family health history of any of the following:
- Breast cancer, especially at a younger age
- Triple-negative breast cancer at age 60 or younger in women
- Cancer in both breasts
- Breast cancer in a male relative
- Ovarian, fallopian tube, or primary peritoneal cancer
- Pancreatic cancer
Genetics: Brca1 And Brca2
About 20 to 25 percent of women diagnosed with ovarian cancer have a hereditary tendency to develop the disease. The most significant risk factor for ovarian cancer is an inherited genetic mutation in one of two genes: breast cancer gene 1 or breast cancer gene 2 . These genes are responsible for about 10 to 15 percent of all ovarian cancers.
Eastern European women and women of Ashkenazi Jewish descent are at a higher risk of carrying BRCA1 and BRCA2 mutations.
Since these genes are linked to both breast and ovarian cancer, women who have had breast cancer have an increased risk of ovarian cancer. You can find more detail about BRCA1 and BRCA2 mutations in the Ovarian Cancer Risk Consensus StatementBRCA1 and BRCA2, which the Alliance endorsed in 2012.
Learn about genetic counseling and testing.
Also Check: What Is The History Of Breast Cancer
Breast And Ovarian Cancer: Is There A Connection
Knowledge is power when it comes to understanding breast cancer. Being armed with the facts can help you make important decisions about your health.
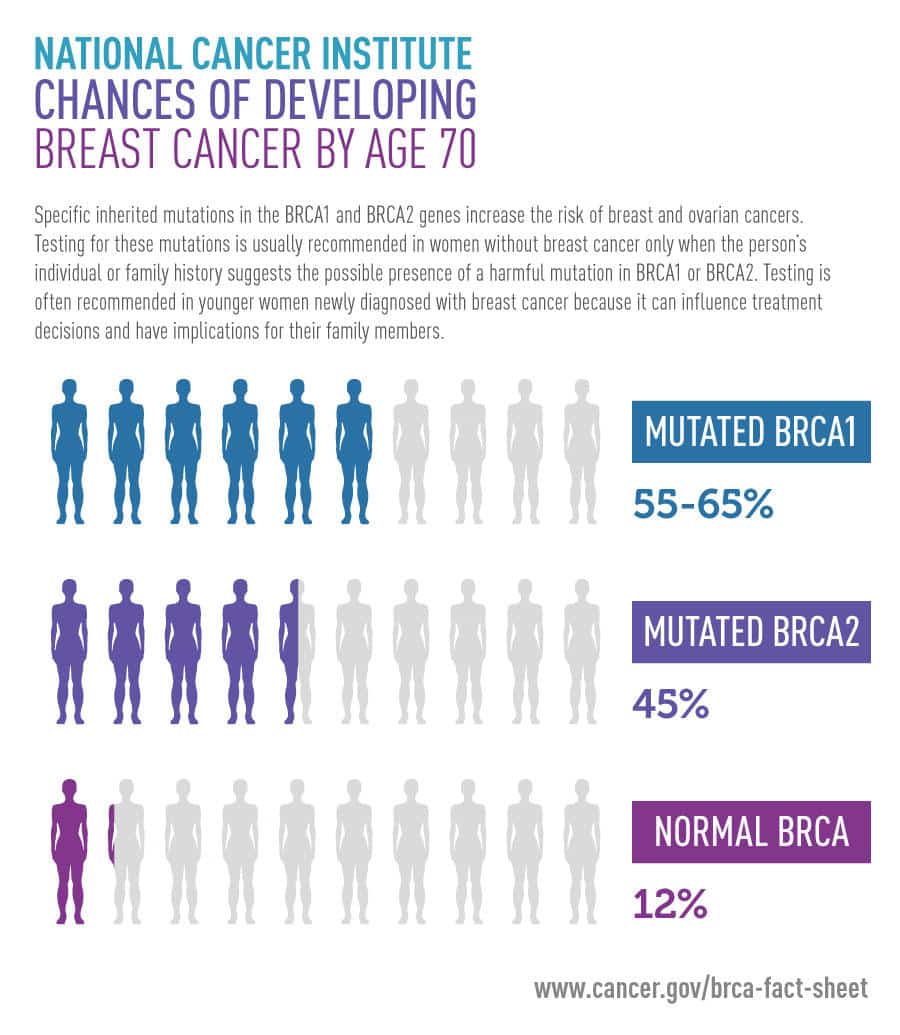
Breast cancer is the most common cancer women face, other than skin cancer. One in 8 women, or about 12%, may develop breast cancer over her lifetime. Ovarian cancer is far less common, with a lifetime risk for the general population of just 2%.
About 5-10% of breast cancers are attributed to genetic mutations, such as BRCA1 or BRCA2. One in 400 women have the BRCA mutation, making their chances of developing breast and ovarian cancer much greater, says Dr. Candy Arentz, breast surgeon at Houston Methodist Cancer Center.
Lowering Risk Of Ovarian Cancer
People with breast cancer who are concerned about their ovarian cancer risk should talk to their doctor to learn more about potential next steps. You may be able to change certain habits in order to lower your risk of developing ovarian cancer in the future. Additionally, you may be a candidate for genetic testing to determine whether you have any inherited gene changes.
Recommended Reading: Minimum Age For Breast Cancer
Risk Factors For Ovarian Cancer
Certain behaviours, substances or conditions can affect your risk, or chance, of developing cancer. Some things increase your risk and some things decrease it. Most cancers are the result of many risks. But sometimes cancer develops in people who don’t have any risks.
Epithelial ovarian carcinoma is the most common type of ovarian cancer. The number of new cases of this cancer increases with age. Most epithelial ovarian carcinomas are found in women who have gone through menopause.
Some people with certain genetic conditions have a higher than average risk for ovarian cancer. Talk to your doctor about your risk. If you have a genetic condition that increases the risk of ovarian cancer, you may need to visit your doctor more often to check for ovarian cancer. Your doctor will recommend what tests you should have and how often you should have them.
The following can increase or decrease your risk for epithelial ovarian carcinoma. The risks for less common types of ovarian cancer are not well known and may not be the same as for epithelial ovarian carcinoma. But epithelial ovarian carcinoma and fallopian tube cancer share many of the same risk factors. Some experts think that this may be because some epithelial ovarian carcinomas can begin in a fallopian tube.
Removal Of The Ovaries And Fallopian Tubes
Women can greatly reduce their risk of ovarian cancer by removing their ovaries and fallopian tubes, a procedure known as prophylactic bilateral salpingo oophorectomy. Primary peritoneal cancer, which is microscopically almost identical to ovarian cancer, can still occur, but is infrequent. One recent study suggests that women with BRCA1 mutations gain the most benefit by removing their ovaries before age 35.
There are risks associated with removing the ovaries and fallopian tubes women should speak to their doctors about whether this procedure is appropriate for them.
You May Like: Side Effects Of Chemo For Breast Cancer
The Link Between Breast And Ovarian Cancer
Women diagnosed with breast cancer are at a higher risk for ovarian cancer. This means that in addition to making decisions around treatment type and location, women must consider what do to about their ovaries. Women who wish to have children face one set of questions, while women who are done with children but not yet menopausal face another.
Genetics and riskSome of the reproductive risk factors for ovarian cancer can also affect breast cancer risk. The risk of ovarian cancer after breast cancer is highest in women with a family history of breast cancer.
About 5 to 10 percent of breast cancers and 10 to 15 of ovarian cancers are hereditary. These hereditary breast and ovarian cancers are caused by a mutation in the BRCA1 or BRCA2 genes. Approximately 30 percent of all breast and ovarian cancer cases are caused by these mutations.
Short- and long-term ovarian suppressionIn premenopausal women, the ovaries make up most of the estrogen in the body. Since estrogen is fuel for growth of hormone-sensitive breast cancer, reducing the amount of estrogen in the body or blocking it may help reduce the risk of recurrence or a secondary cancer such as ovarian.
Ovarian suppression is one way to slow down or block the growth of estrogen production in the ovaries and stops women from having menstrual cycles, says Dr. Igor Medic, a medical oncologist affiliated with Sharp Grossmont Hospital. Ovarian suppression is an option only for women who have yet to enter menopause.
About Inherited Breast And Ovarian Cancer
Breast cancer is one of the most common cancers in the UK. It affects 1 in 8 women and 1 in 870 men during their lifetime.
Ovarian cancer is less common. 1 in 52 women will be diagnosed with ovarian cancer during their lifetime.
Many people have someone in their family who is affected by one of these cancers. Only a small number of cases are clearly linked to inherited cancer genes.
An inherited gene mutation that increases the risk of breast and ovarian cancer is more likely if there is a pattern of cancer in your family. These are examples of patterns:
- One of your first-degree relatives was diagnosed with breast cancer before the age of 40. First-degree relatives are your parents, brothers, sisters and children.
- Several family members have been diagnosed with breast cancer or ovarian cancer.
- A male relative was diagnosed with breast cancer.
- A relative had breast cancer in both breasts .
- You have a family history of cancer and you are from an Eastern European or Ashkenazi Jewish background.
If you are worried about the pattern of cancer in your family, start by talking to your GP. If needed, they will refer you to a genetics specialist.
Read Also: What Stage Of Breast Cancer Requires Chemotherapy
What Happens When Breast Cancer Develops In A Woman Who Carries A Gene Fault
If breast cancer develops in a woman who carries a gene fault the treatment choices are the same as they are for any woman. Treatment may include mastectomy or breast conservation surgery. Radiotherapy, chemotherapy and/or hormone therapy may also be recommended. Your treatment team may be more likely to recommend a mastectomy or may even recommend removing both breasts if you carry a gene fault. This is because your risk of developing a breast cancer in the other breast in the future is higher than it is for other women.
The treatment for breast cancer depends on lots of factors and these will be discussed in detail with you if this situation develop
What Is Hereditary Breast And Ovarian Cancer
A diagnosis of Hereditary Breast and Ovarian Cancer Syndrome is considered when there are multiple cases of breast cancer and/or ovarian cancer on the same side of the family. The chance that a family has HBOC increases in any of these situations:
-
1 or more women are diagnosed at age 45 or younger
-
1 or more women are diagnosed with breast cancer before age 50 with an additional family history of cancer, such as prostate cancer, melanoma, and pancreatic cancer
-
There are breast and/or ovarian cancers in multiple generations on the same side of the family, such as having both a grandmother and an aunt on the fathers side both diagnosed with these cancers
-
A woman is diagnosed with a second breast cancer in the same or the other breast or has both breast and ovarian cancers
-
A male relative is diagnosed with breast cancer
-
There is a history of breast cancer, ovarian cancer, prostate cancer, and/or pancreatic cancer on the same side of the family
-
Having Ashkenazi Jewish ancestry
Don’t Miss: Can You Have Breast Cancer In Both Breast
Genetic Testing For Hereditary Breast And Ovarian Cancer
Genetic testing is available for hereditary breast and ovarian cancer. Most breast and ovarian cancer is not caused by inherited mutations, so genetic testing will not help most women with a family health history of breast and ovarian cancer. Genetic testing will not identify the cause for some hereditary breast and ovarian cancers, because the genes affected in these cancers are not yet known.
Genetic counseling before genetic testing for hereditary breast and ovarian cancer is important to determine whether you and your family are likely enough to have a mutation that it is worth getting tested. Usually, genetic testing is recommended if you have:
- A strong family health history of breast and ovarian cancer
- A moderate family health history of breast and ovarian cancer and are of Ashkenazi Jewish or Eastern European ancestry
- A personal history of breast cancer and meet certain criteria
- A personal history of ovarian, fallopian tube, or primary peritoneal cancer
- A known BRCA1, BRCA2, or other inherited mutation in your family
The BRCA1 and BRCA2 genes
Genetic counseling after genetic testing is important to help you understand your test results and decide the next steps for you and your family: