Types Of Breast Cancer
There are several different types of breast cancer, which develop in different parts of the breast.
Breast cancer is often divided into either:
- non-invasive breast cancer found in the ducts of the breast which has not spread into the breast tissue surrounding the ducts. Non-invasive breast cancer is usually found during a mammogram and rarely shows as a breast lump.
- invasive breast cancer where the cancer cells have spread through the lining of the ducts into the surrounding breast tissue. This is the most common type of breast cancer.
Other, less common types of breast cancer include:
- invasive lobular breast cancer
- inflammatory breast cancer
It’s possible for breast cancer to spread to other parts of the body, usually through the blood or the axillary lymph nodes. These are small lymphatic glands that filter bacteria and cells from the mammary gland.
If this happens, it’s known as secondary, or metastatic, breast cancer.
How Quickly Breast Cancer Develops
The actual time it takes for breast cancer to grow from a single cancer cell to a cancerous tumor is unknown. Part of the reason is that estimates based on doubling time assume that the rate stays constant at all times as the tumor grows.
If this were true, cancer with a doubling time of 200 days would take 20 years to develop into a detectable tumor. A doubling time of 100 days would take 10 years to be found on exam. In contrast, a breast tumor with a doubling time of 20 days would take only 2 years to develop.
Most studies have found the average doubling time to be between 50 days and 200 days. This means it’s possible that breast cancers diagnosed now began at least 5 years earlier, but again, this assumes the growth rate is constant. It is not.
Coverage Of Breast Cancer Screening And Prevention Services
Among women in the United States, breast cancer is the most commonly diagnosed cancer and the second leading cause of cancer death. In 2016, an estimated 3.5 million women in the U.S. were living with breast cancer. The Affordable Care Act and many state laws have provisions that assure that most women with private insurance, Medicaid, and Medicare have coverage for breast cancer screening services. This typically includes screening mammography for the general population of women, but also can include genetic testing and preventive medications for high-risk women over the age of 35. This factsheet discusses breast cancer screening and prevention services, and reviews the scope of private and public insurance coverage, as well as access to those services for women in the US.
You May Like: How Long After Breast Cancer Diagnosis Does Treatment Start
Primary And Adjunctive Screening In Women With Dense Breasts
The USPSTF found insufficient evidence to assess the balance of benefits and harms of adjunctive screening for breast cancer using breast ultrasonography, MRI, DBT, or other methods in women identified to have dense breasts on an otherwise negative screening mammogram.
Epidemiology of Dense Breasts
In the United States, the most commonly used classification system for breast density is the American College of Radiologys Breast Imaging Reporting and Data System 4-category scale . Data from the BCSC indicate that about 25 million women aged 40 to 74 years are classified as having heterogeneously or extremely dense breasts. The proportion of women with dense breasts is highest among those aged 40 to 49 years and decreases with age.14
Increased breast density is a risk factor for breast cancer. Data from the BCSC indicate that, compared with women with average breast density, women aged 40 to 49 years with heterogeneously or extremely dense breasts have a relative risk of 1.23 for developing invasive breast cancer. For women aged 50 to 64 years with heterogeneously or extremely dense breasts, the RR is 1.29, and for women aged 65 to 74 years, it is 1.30.7 However, women with dense breasts who develop breast cancer do not have an increased risk for dying from the disease, after adjustment for stage, treatment, method of detection, and other risk factors, according to data from the BCSC.15
Primary Screening Test Performance Characteristics
Primary Screening Frequency
Assessment
How Often To Screen
Once a woman has decided to begin screening, the next decision is how often to undergo screening. No clinical trials compared annual mammography with a longer interval in women of any age. In the randomized trials that demonstrated the effectiveness of mammography in reducing breast cancer deaths in women aged 40 to 74 years, screening intervals ranged from 12 to 33 months.2, 3 There was no clear trend for greater benefit in trials of annual mammography, but other differences between the trials preclude certainty that no difference in benefit exists. Available observational evidence evaluating the effects of varying mammography intervals found no difference in the number of breast cancer deaths between women aged 50 years or older who were screened biennially versus annually.2, 3
Regardless of the starting age for screening, the models consistently predict a small incremental increase in the number of breast cancer deaths averted when moving from biennial to annual mammography, but also a large increase in the number of harms .7, 8 The USPSTF concludes that for most women, biennial mammography screening provides the best overall balance of benefit and harms.
You May Like: How Would I Know If I Had Breast Cancer
Response To Public Comment
A draft recommendation statement was posted for public comment on the USPSTF Web site from 21 April through 18 May 2015. In response to the comments received, the USPSTF clarified certain terminology , updated or added references , and provided additional context around the potential risks of radiation exposure due to mammography screening. Additional discussion of the public comments is below.
Benefits of Contemporary Screening Mammography
Screening Mammography in Women Aged 40 to 49 Years
Some commenters incorrectly believed that the C recommendation for women aged 40 to 49 years represented a change from what the USPSTF had recommended in the past. Others thought that the C recommendation meant that the USPSTF was recommending against screening in this group of women. As noted previously, the recommendation for women aged 40 to 49 years was also a C in 2009 . This update clarifies the language around what the C recommendation means. It is not a recommendation against screening but a statement that the decision to undergo screening mammography for women in their 40s should be an informed, individual one, after she weighs the potential benefit against the potential harms.
Screening Mammography in Women Aged 70 to 74 Years or Older
Definition of Overdiagnosis
DBT
Comparison of the USPSTFs Recommendations With Those of Other Organizations
Insurance Coverage and Access to Mammography
Teen Breast Cancer Causes And Symptoms
There are times that teen girls may discover a small lump in their breast, but it is almost always benign and typically triggered by normal hormonal fluctuations. These noncancerous lumps usually go away on their own. However, there are symptoms a doctor should be made aware of:
- The breast tissue hurts outside of normal soreness caused by a menstrual period
- Breast tissue puckers or dimples
- Itchy or scaly rash on breast
- Unexplained changes in breast symmetry, shape, and size
- Breast swelling, red, or hot to touch
- Nipple discharge is liquid or bloody
- Lump spreads to armpit or collarbone
- Lump is hard
- Lump is painful
- Lump is fixed to the chest wall
Due to the high amount of treatment options for teen breast development, the survival rate is high. Teenagers are healthy enough to tolerate the most aggressive therapies used to treat breast cancer. Thats why its best to avoid high-risk lifestyle behaviors that can increase this risk. The American Cancer Society has noted that although environmental and lifestyle behaviors are not strongly associated with breast cancer, its best to avoid engaging in risky ones like smoking and consistently unhealthy diets. Other behaviors like radiation exposure to treat other diseases like leukemia or Hodgkins disease in young girls can increase the risk of breast cancer development, which takes an average of 20 years to develop.
Don’t Miss: Is Grade 3 Breast Cancer Serious
Category A: Eligible For Direct Entry Into The High Risk Breast Screening Program Based On Personal And Family History
Must meet one of the following risk criteria:
- Known carrier of a gene mutation
- First degree relative of a carrier of a gene mutation , has previously had genetic counselling, and has declined genetic testing
- Previously assessed by a genetic clinic as having an equal to or greater than 25% personal lifetime risk of breast cancer based on family history
- Received radiation therapy to the chest before age 30 and at least 8 years ago
Colon And Rectal Cancer And Polyps
For people at average risk for colorectal cancer, the American Cancer Society recommends starting regular screening at age 45. This can be done either with a sensitive test that looks for signs of cancer in a persons stool , or with an exam that looks at the colon and rectum . Talk to your health care provider about which tests might be good options for you, and to your insurance provider about your coverage. No matter which test you choose, the most important thing is to get screened.
If youre in good health, you should continue regular screening through age 75.
For people ages 76 through 85, talk with your health care provider about whether continuing to get screened is right for you. When deciding, take into account your own preferences, overall health, and past screening history.
People over 85 should no longer get colorectal cancer screening.
If you choose to be screened with a test other than colonoscopy, any abnormal test result needs to be followed up with a colonoscopy.
You May Like: What Is Breast Cancer Like
Estimate Of Magnitude Of Net Benefit
Digital breast tomosynthesis is an emerging technology for breast cancer screening. Preliminary evidence suggests that it can reduce recall rates for false-positive results and detect more cancer compared with conventional digital mammography. However, it may increase breast biopsy rates, and as currently practiced in most settings, DBT exposes women to more radiation than conventional 2-dimensional mammography. It is not clear whether all of the extra cancer cases detected by DBT actually represent a benefit . Most importantly, no studies assessed the effect of DBT on important health outcomes for women, such as quality of life, morbidity, or mortality. Finally, increased breast density is a common condition that imparts some increased risk for breast cancer, and it reduces the test performance characteristics of mammography as well. Current evidence on the use of adjunctive screening in women with increased breast density is not sufficient to recommend a specific screening strategy. These are important areas for future research.
Benefit And Harms Of Screening And Early Treatment
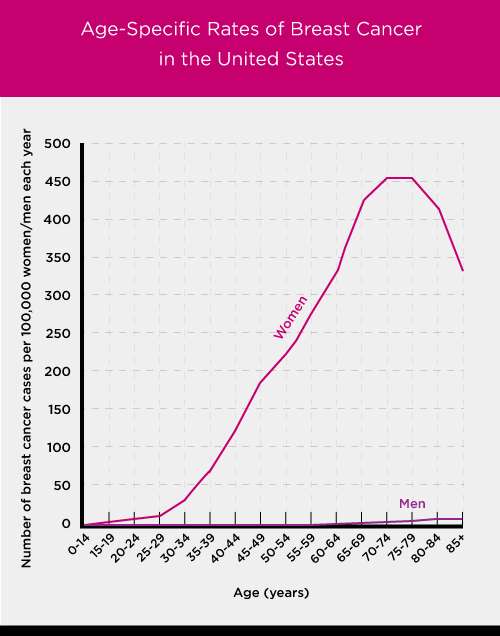
The USPSTF found adequate evidence that mammography screening reduces breast cancer mortality in women aged 40 to 74 years. The number of breast cancer deaths averted increases with age women aged 40 to 49 years benefit the least and women aged 60 to 69 years benefit the most. Age is the most important risk factor for breast cancer, and the increased benefit observed with age is at least partly due to the increase in risk. Women aged 40 to 49 years who have a first-degree relative with breast cancer have a risk for breast cancer similar to that of women aged 50 to 59 years without a family history. Direct evidence about the benefits of screening mammography in women aged 75 years or older is lacking.
The USPSTF found adequate evidence that screening for breast cancer with mammography results in harms for women aged 40 to 74 years. The most important harm is the diagnosis and treatment of noninvasive and invasive breast cancer that would otherwise not have become a threat to a womans health, or even apparent, during her lifetime . False-positive results are common and lead to unnecessary and sometimes invasive follow-up testing, with the potential for psychological harms . False-negative results also occur and may provide false reassurance. Radiation-induced breast cancer and resulting death can also occur, although the number of both of these events is predicted to be low.
Don’t Miss: What Does Invasive Breast Cancer Mean
Breast Cancer Vs Normal Development
Normal breast development can resemble breast cancer, and it is not possible to tell what is normal and what is not based on a comparison of symptoms.
Normal breast development, however, usually follows a pattern. It begins with nickel-sized lumps under each nipple, and the breasts gradually grow from these lumps.
Breast cancer, in general, is survivable with prompt treatment. This is particularly true of noninvasive breast cancers, and of breast cancers that have not spread to other areas of the body.
Treatments often include chemotherapy, radiation, medication, surgery, or a combination of these.
Breast Cancer Treatment In Teens

Treatment for breast cancer in teens depends on how far the disease has spread and the teens general health and personal circumstances. All of these factors play an important role in what steps are taken. Some of the treatment options include:
- Surgery In these cases, a lumpectomy or mastectomy is conducted. A lumpectomy includes the removal of the tumor and surrounding tissue. A mastectomy involves the removal of the whole breast. Depending on how far the disease has spread, either option may be best.
- Radiation This therapy is usually used following a lumpectomy. Using cancer-killing beams, radiation therapy targets undetected cancer cells further reducing the risk of cancer returning.
- Hormone This therapy is effective for those breast cancers that are affected by hormones in the blood. It utilizes drugs that block estrogen and/or progesterone.
- Chemotherapy This is usually administered after breast surgery but before radiation, and uses drugs directly injected into the vein via a needle or pill to target and kill cancer cells.
Don’t Miss: How Long Do You Have With Stage 4 Breast Cancer
Research Needs And Gaps
Trial data are too limited to directly inform the question of what the best screening strategy is for women or how clinicians can best tailor that strategy to the individual.
Overdiagnosis and resulting overtreatment of breast cancer that would otherwise not have become a threat to a womans health during her lifetime is the most important harm associated with breast cancer screening. Because it is impossible to determine for any individual patient whether a diagnosed cancer will or will not progress, measurements of overdiagnosis are not straightforward but rather are indirectly quantified. Current estimates of the magnitude of overdiagnosis associated with mammography screening vary widely. Researchers in the field must work together to critically evaluate and ultimately agree on uniform definitions and standards to optimally measure and monitor overdiagnosis and overtreatment in breast cancer screening programs.
Most of the available screening trials and high-quality cohort studies were performed in Europe and predominately enrolled white women younger than age 70 years. Direct evidence about any differential effectiveness of breast cancer screening is lacking for important subgroups of women, such as African American women, who are at increased risk for dying of breast cancer, and older women, for whom balancing the potential benefits and harms of screening may become increasingly challenging with advancing age.
What Are The Risks Of Having A Mammogram
Each time you have a mammogram, there is a risk that the test:
- May miss some breast cancers. And some cancers that are found may still be fatal, even with treatment.
- May show an abnormal result when it turns out there wasn’t any cancer . This means you may need more testssuch as another mammogram, a breast ultrasound, or a biopsyto make sure you don’t have cancer. These tests can be harmful and cause a lot of worry.
- May find cancers that will never cause a problem . Some breast cancers never grow or spread and are harmless. You might have this type of cancer, but a mammogram can’t tell whether it’s harmless. So you may get cancer treatmentincluding surgery, radiation, or chemotherapythat you don’t need.
- Will briefly expose you to very small amounts of radiation. While the risk from being exposed to radiation from a mammogram is low, it can add up over time.
| Ages 4049 | About 19 out of 1,000 women |
|---|---|
| Ages 5059 | About 30 out of 1,000 women |
| Ages 6069 | About 44 out of 1,000 women |
*Based on the best available evidence
*Based on the best available evidence
Breast cancer diagnosis
Mammograms can find some breast cancers early, when the cancer may be more easily treated. Often a mammogram can find cancers that are too small for you or your doctor to feel.
Take a group of women who have a mammogram every year for 10 years.footnote 1
Survival
Risks
Understanding the evidence
You May Like: Could I Have Breast Cancer
Effectiveness Of Early Detection And Treatment
Primary Screening With Conventional Mammography
An updated meta-analysis by Nelson and colleagues of RCTs of screening mammography found similar RR reductions in breast cancer mortality by age group as the previous USPSTF evidence review. The combined RRs were 0.92 for women aged 39 to 49 years, 0.86 for women aged 50 to 59 years, 0.67 for women aged 60 to 69 years, and 0.80 for women aged 70 to 74 years.2, 3
None of the trials nor the combined meta-analysis demonstrated a difference in all-cause mortality with screening mammography.2
Observational studies of screening mammography reported a wide range of breast cancer mortality reduction rates. Recent meta-analyses from the EUROSCREEN Working Group showed an approximate 25% to 31% relative reduction in breast cancer deaths in women aged 50 to 69 years who were invited to screening. In comparison, meta-analysis of RCTs that used an intention-to-treat analysis found a 19% to 22% breast cancer mortality reduction in women in the same age range.2, 3
Primary Screening With DBT
No studies evaluated the effect of screening for breast cancer with DBT on important health outcomes, such as mortality, treatment-related morbidity, or quality of life.13
Adjunctive Screening in Women With Dense Breasts
No studies evaluated the effects of adjunctive screening with any method in women with dense breasts on breast cancer rates, quality of life, or mortality.17, 18