Individualized Prediction Of Survival Benefit From Locoregional Surgical Treatment For Patients With Metastatic Breast Cancer
- 1Department of Breast and Thyroid Surgery, Zhejiang Provincial People’s Hospital, People’s Hospital of Hangzhou Medical College, Hangzhou, China
- 2Department of Breast Surgery, The First Affiliated Hospital, College of Medicine, Zhejiang University, Hangzhou, China
- 3Department of General Surgery, The 7th Affiliated Hospital of Sun Yat-sen University, Shenzhen, China
Objective: Recently, performing locoregional surgical treatment still remains debatable in patients with metastatic breast cancer . Current study aimed to develop prognostic nomograms for predicting the long-term survival in MBC patients with or without surgical intervention, thereby assisting clinicians in making individualized choice.
Methods: The training set included 5173 patients who were diagnosed with MBC in 20102013 from the Surveillance, Epidemiology, and End Results Program, while the validation set comprised 2924 patients diagnosed in 20142015. Multivariant Cox hazard model was applied to determine the independent risk factors for overall survival and breast cancer specific survival . Then, individualized pre- and postoperative nomograms for predicting 1- or 3-year survival probabilities were constructed accordingly. Internal and external validations were conducted to determine the accuracy of these nomograms by calculating concordance index and plotting calibration curves.
What Other Therapies Are Helpful For Reducing Complications
A number of therapies are commonly used in patients with metastatic breast cancer to treat, prevent or reduce complications.
Supportive care
Anemia
Treatment with erythropoiesis stimulating agents is indicated only in patients in which treatment is administered without a curative intent. Most patients with metastatic breast cancer fall in to this category.
Caution using these agents is recommended as they are associated with an increased risk of thromboembolic events. When they are used, the target hemoglobin should never be at supranormal levels. In symptomatic patients, transfusion of leukoreduced packed red blood cells provides rapid relief of symptoms.
Neutropenia
Primary prophylaxis with growth factor support is not commonly used in patients with metastatic breast cancer. As a general rule, quality of life with close attention to the side effects of chemotherapy is a priority of treatment. However, in patients with poor bone marrow reserve after prolonged chemotherapy treatments or with history of neutropenic fever, filgastrim or pegfilgrastim can be used.
Nausea/vomiting
Some chemotherapeutic agents used in the metastatic setting are moderately to highly ematogenic. Medications for the prevention of acute nausea should be administered concurrently with chemotherapy and shortly thereafter. 5-HT3 antagonists such as ondansetron, granisetron, or palonosetron are recommended.
Palmar-Plantar erythrodysesthesia
Bone metastases
Surgery
Objective Response To First
Out of the 950 patients that received at least one line of treatment, 70 had a radiologically complete response and 343 patients had a PR for an ORR to first-line treatment of 43.5% . In contrast, 273 patients had SD as best response and 192 patients had disease progression at first assessment. The remaining patients had either no evidence of disease or no evaluable information . An objective response was achieved by 51.0% of patients treated with first-line chemotherapy compared to 32.2% of those treated with first-line endocrine therapy . However, rates of PD as best response on first-line treatment were similar between the two groups .
Responders at first line had improved PFS at first line compared to nonresponders but not at second line . At the time of data cutoff, 192 patients with an objective response at first line and 255 patients with SD or PD had died. Median OS was significantly longer for patients that had an objective response the corresponding median OS was 61.9 months for responders versus 41.3 months for nonresponders . In multivariable analysis, failure to achieve an objective response to first-line treatment was an independent predictor of poor survival outcome, when adjusted for ER status, HER2 status, age, site of metastasis, type of first-line therapy, and disease-free interval .
Table 3.
Multivariable Cox regression analysis for overall survival in the 651 patients with available data
Fig. 2.
You May Like: Can Shingles Cause Breast Cancer
Read Also: How Long Chemotherapy For Breast Cancer
Recurrence Of Metastatic Breast Cancer
Metastatic breast cancer is considered a chronic disease, so it doesnt go away and recur.
But in recent years, people under age 50 have seen a particularly strong decline in death rates due to breast cancer, according to the Centers for Disease Control and Prevention .
These declines are due in part to improved screening and treatment for the disease.
There are a few general facts that are helpful to know about breast cancer outlook:
- Breast cancer is the most common cancer diagnosis in the United States, according to the
What Should You Tell The Patient And The Family About Prognosis
A pivotal component of the management of patients with metastatic breast cancer is the discussion of goals of care. Despite important advances in the treatment, metastatic breast cancer remains, as a general rule, an incurable disease. Median survival is 2 years and 5-year overall survival estimates range from 17-28%.
Patients with bone-only disease tend to have better prognosis than patients with visceral disease patients with uncontrolled brain metastases have very poor prognosis. Patients with bone-only disease can have median survival of up to 5 years or more, compared with patients with brain metastases who tend to live less than 12 months.
Without treatment, median survival ranges 9 to 12 months. Among treated patients, responses and clinical outcomes depend on a number of factors, including the breast cancer tumor subtype, the patientâs performance status, the number and extension of the metastases, the disease-free interval, and prior therapies received, among others.
In rare instances , long-term remissions can be achieved. It is not possible to predict which individuals will fall into this group. They tend to be young, have good performance status and very low volume of disease. Also, in patients with solitary metastases, complete responses can be achieved and in few cases a multidisciplinary treatment approach with curative intent can be justified.
Copyright © 2017, 2013 Decision Support in Medicine, LLC. All rights reserved.
Recommended Reading: Can You Get Breast Cancer In Your 20s
What Is Metastatic Breast Cancer
Metastatic breast cancer is also called stage IV or advanced breast cancer, in which the cancer has spread beyond the breast and adjacent lymph nodes to other parts of the body such as the bones, lungs, liver, or brain.
Remote recurrence occurs when metastatic breast cancer develops months or years after a person has finished therapy for early or locally advanced breast cancer.
Only 6% of women and 9% of men in the U.S. are diagnosed with de novo metastatic breast cancer, which refers to breast cancer that is already metastatic at the time of diagnosis.
What Therapies Should You Initiate Immediately Ie Emergently
Most cases of metastatic breast cancer do not require urgent initiation of treatment however, in rapidly growing tumors, therapy should be initiated promptly. Furthermore, a number of disease-related complications may need to be identified and addressed emergently.
Spinal cord compression
Treatment with corticosteroids should be started. A clear dose schedule has not been determined one option is to administer dexamethasone 10 mg IV or 16 mg PO followed by 4 mg IV or PO every 6 hours. Radiation oncology and spine surgery consultations should be requested immediately.
Brain metastases
Initiate steroids as recommended for spinal dose compression. Consultation with neurosurgery and radiation oncology is mandatory to select the best treatment modality
Superior vena cava syndrome
Consider steroids and treat with radiation therapy. In specific cases a stent can be considered. Chemotherapy has been used in highly proliferative disease, especially if there is a history of radiotherapy resistance.
Pericardial effusion
Occurs secondary to tumor involvement and can lead to cardiac tamponade. Pericardiocentesis or a pericardial window is indicated. In patients with poor performance status, radiation therapy may provide benefit.
Hypercalcemia
Pain crisis
Visceral crisis
In patients with important visceral involvement who can tolerate treatment, systemic chemotherapy in combination with targeted therapy if indicated should be started promptly.
Read Also: What Type Of Radiation Is Used For Breast Cancer
De Novo Stage Iv Breast Cancer
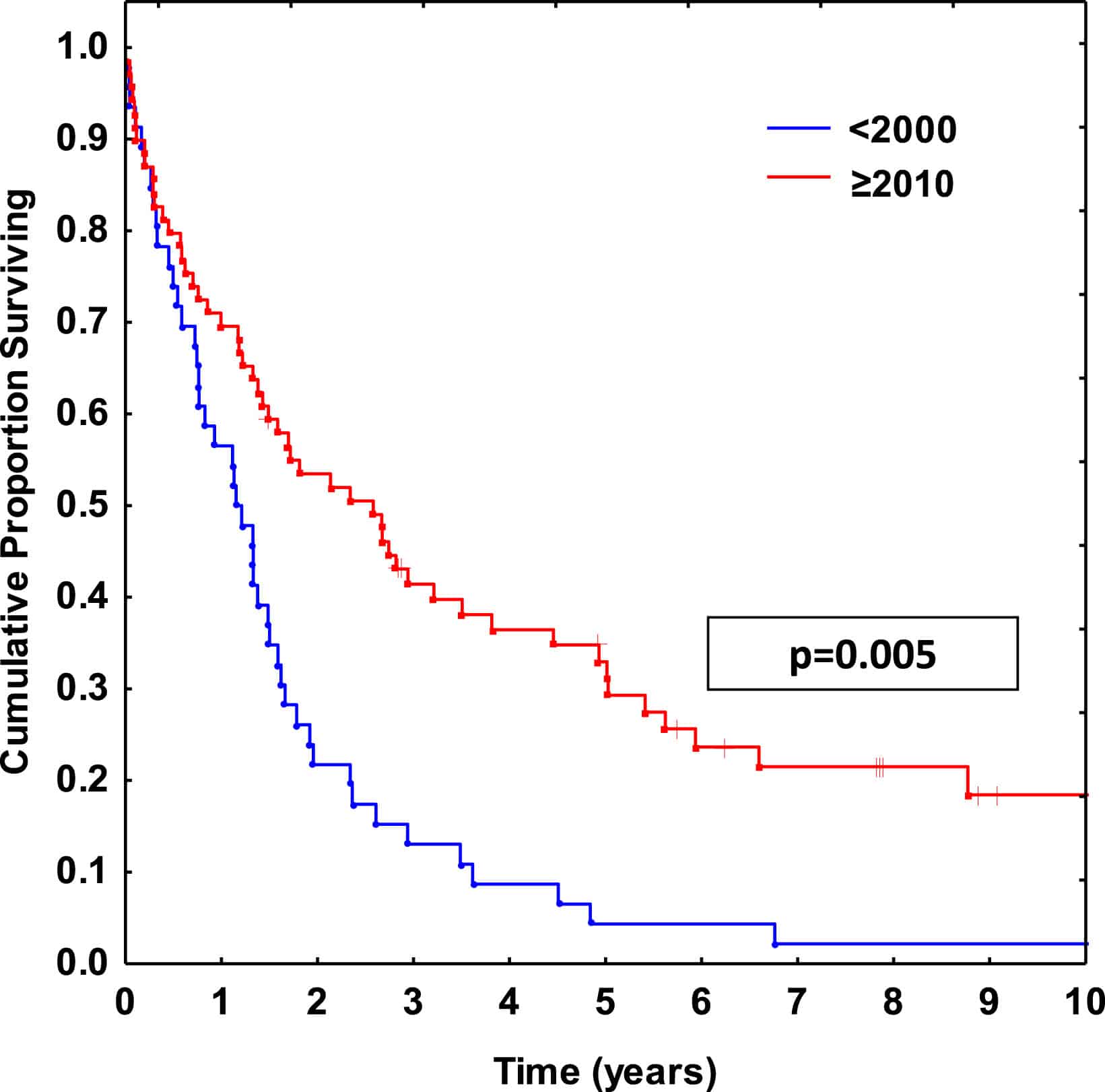
We identified eight studies that assessed survival improvement in exclusively de novo stage IV disease . These included registry-based studies and single- or multi-institution studies . Meta-regression found no statistically significant improvement from 1980 to 1990 but statistically significant improvement thereafter . We estimated median unadjusted survival to have been 19 months in 1980, 20 months in 1990, 23 months in 2000, and 31 months in 2010 . Only one of these studies reported survival separately for ER-positive and ER-negative disease and showed improvement for ER-positive disease but not ER-negative disease from 1987 to 2000. Multivariable analysis was performed in four of the six studies: the association between time period of diagnosis and survival persisted after multivariable analysis in three of the four studies .
What Are The Symptoms Of Metastatic Cancer
The symptoms produced by metastatic breast cancer vary depending on the location of the metastases.
For example, metastatic disease to the bone causes severe, progressive pain, and less commonly, pathological fracture, erythema over the affected bone and swelling.
Breast cancer cells that have spread to the brain cause persistent, progressively worsening headache, visual changes, seizures, nausea, vomiting, vertigo, behavioral and personality changes and increased intracranial pressure.
Metastatic disease to the liver causes jaundice, elevated liver enzymes, abdominal pain, loss of appetite, nausea, and vomiting.
Metastatic breast cancer to the lung or pleura causes chronic cough, dyspnea, abnormal chest x-ray, and chest pain.
In addition, general, non-specific systemic symptoms of metastatic breast cancer include fatigue, malaise, weight loss and poor appetite.
You May Like: Trastuzumab Deruxtecan In Previously Treated Her2-positive Breast Cancer
Encouraging Statistics On Prognosis Of Metastatic Breast Cancer
In recent years, there have been some encouraging new statistics on the prognosis of metastatic breast cancer, these include:
- The statistics on survival rates show that women with breast cancer live longer today than ever before.
- In the past decade, the survival rate has substantially increased, due to an improvement in early diagnosis and screening, as well as improved targeted treatment.
- Survival rates are higher for women in higher economic groups
- The stage of cancer at the time of diagnosis plays an impactful role in prognosis, the highest survival rate begins for those who are five years post-treatment.
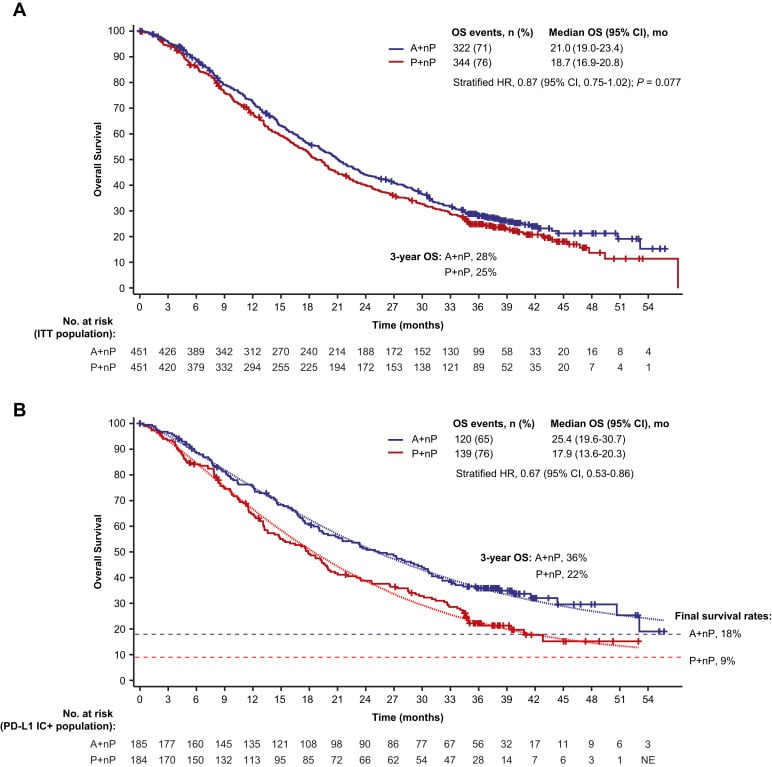
Using Cdk4/6 Inhibitors As A First
Some oncologists still often reserve CDK4/6 inhibitors as a second-line treatment for their patients with advanced breast cancer, waiting until the disease has started to progress on hormone-blocking therapies. But Dr. Burris said he hopes this thinking will now change.
We shouldnt be saving these therapies, Dr. Burris said. Regardless of which you pick, oncologists should be offering patients these drugs as a first-line treatment.
There doesnt appear to be a consensus on whether the updated findings from MONALEESA-2 mean ribociclib should be the preferred initial treatment.
Dr. Burris pointed to similar overall survival improvements seen with ribociclib in two other large clinical trials involving people with advanced breast cancer: MONALEESA-3 and MONALEESA-7, in younger, premenopausal patients.
Because of his long involvement in clinical trials of ribociclib and the consistency of the survival data from these trials, Dr. Burris said that he tends to favor it for many of his patients.
Other oncologists are likely to take the MONALEESA-2 results as confirmation that any of the CDK4/6 inhibitors are a good choice, Dr. McShane said.
Overall survival data from large clinical trials of palbociclib and abemaciclib as a first-line treatment in postmenopausal women with HR-positive, HER2-negative advanced breast cancer are expected to be available soon, Dr. McShane said, and she expects that they will also show an improved overall survival with the CDK4/6 inhibitor.
Recommended Reading: How To Remove Breast Cancer
Triple Negative Breast Cancer
With this type of breast cancer, the breast cancer cells dont have ER+ or PR+ receptors. They dont overproduce the HER2 protein, so hormone therapy isnt very effective.
Instead, triple negative stage 4 breast cancer is usually treated with chemotherapy. Radiation therapy may also be an option, depending on the site of metastasis.
Risk Covariates Related With Survival In Cohorts With And Without Surgery
Initially, univariate Cox proportional models regarding to groups with and without surgery were built, respectively, to evaluate the multiple factors related with OS and BCSS . Eleven parameters were incorporated into this Cox model, including one demographic variable, seven disease-related variables, and three treatment-related variables. As shown in Table 3, the risk of death increased dramatically with age both in cohort with and without surgery. The T staging exerted a significant prognostic factors. For patients not receiving surgery, the risk of death in patients with higher T stage was higher than those with T1 tumors expect T2 tumors. Meanwhile, among patients receiving surgery, T staging was consistently associated with worse OS and BCSS compared with T1 . The risk of death also increased in patients with poorer tumor differentiation. Patients with lung, brain or multiple sites involvement had a significantly higher risk of death than those with only bone metastases regardless of surgery or not . However, there was no correlation between higher N staging and poorer survival outcomes in both groups. Moreover, positive status of ER, PR and HER2, and treatments with radiation and chemotherapy were proved to be protective factors for better OS and BCSS in both surgery and non-surgery group. Intriguingly, patients received radical mastectomy had slightly better prognosis than those undergone lumpectomy or mastectomy both in OS and BCSS .
Don’t Miss: Is Inflammatory Breast Cancer Hereditary
Study Design And Endpoints
This is a retrospective cohort study whose dual objective was to investigate the efficacy of later treatment lines for MBC in terms of objective response rate , progression-free survival , and OS and to evaluate the association between response to first-line therapy and long-term survival. This noninterventional retrospective study was approved by the responsible ethics committee .
Within the scope of this study, ORR was defined as the proportion of patients achieving complete response and partial response . Progressive disease was defined as an increase in tumor lesions or the appearance of new ones, while stable disease included cases not defined as either PR or PD. The assessment of radiologic response was performed by the treating physician according to local practice, which was largely consistent with the initial version of the Response Evaluation Criteria In Solid Tumors . For each treatment line, the best radiologic response was documented, regardless of when that was achieved. PFS was defined as the time from initiation of treatment until the time of documentation of disease progression or death, whichever occurred first. OS was defined as the time from diagnosis of MBC until the time of death from any cause or the date of last follow-up.
Patients And Data Collection
Women aged 18 years and above, diagnosed with MBC during the period of January 1st, 2005 to December 31st, 2016, were identified through the SBCR. This is a population-based registry in which cases of BC diagnosed in the StockholmGotland area, Sweden have been reported since 1976. It contains both demographic and clinicopathological data and is a part of the national breast cancer registry which has been shown to have excellent cover . Cases of relapse/metastasis are reported by the clinician and/or pathologist. In addition, identification of non-reported cases is done yearly in the registry by manually checking the presence of metastatic diagnosis in all patients with breast cancer as cause of death in the Swedish death registry. The date of diagnosis was defined as the time of diagnosis of metastatic disease, verified either through histology, cytology, or imaging, whichever came first. For cutaneous metastases, the date of the clinical diagnosis by the physician was accepted.
Exclusion criteria from the study cohort were histology or cytology showing other metastatic cancer besides BC, concurrent metastatic cancer in addition to MBC and death occurring more than 90 days from MBC diagnosis. End of follow-up was set to Dec 31st, 2017.
Recommended Reading: Why Is Breast Cancer Screening Important
De Novo And Recurrent Metastatic Breast Cancer A Systematic Review Of Population
- AffiliationsThe School of Medicine, University of Notre Dame Australia, Darlinghurst, AustraliaThe National Health and Medical Research Council Clinical Trials Centre, The University of Sydney, Camperdown, AustraliaNHMRC Centre of Research Excellence in Medicines Intelligence, Australia
- DL O’ConnellAffiliationsThe Daffodil Centre, The University of Sydney, a joint venture with Cancer Council NSW, Sydney, AustraliaSchool of Medicine and Public Health, College of Health, Medicine and Wellbeing, The University of Newcastle, Australia
- BE KielyAffiliationsThe National Health and Medical Research Council Clinical Trials Centre, The University of Sydney, Camperdown, Australia
- NHMRC Centre of Research Excellence in Medicines Intelligence, AustraliaMedicines Policy Research Unit, Centre for Big Data Research in Health, UNSW Sydney, Australia
- NHMRC Centre of Research Excellence in Medicines Intelligence, AustraliaMedicines Policy Research Unit, Centre for Big Data Research in Health, UNSW Sydney, Australia
- MK BulsaraAffiliations
- N HoussamiAffiliations
Why Does Metastatic Breast Cancer Happen
Most often, metastatic cancer occurs because treatment didnt destroy all the cancer cells. Sometimes, a few cells remain dormant, or are hidden and undetectable. Then, for reasons providers dont fully understand, the cells begin to grow and spread again.
De novo metastatic breast cancer means that at the time of initial diagnosis, the breast cancer has already spread to other parts of the body. In the absence of treatment, the cancer spreads.
There is nothing you can do to keep breast cancer from metastasizing. And metastatic breast cancer doesnt happen because of something you did.
Recommended Reading: Breast Cancer And Hair Dye
Mechanisms Of Breast Cancer Metastasis
No one really knows what factors will make a certain patient more or less susceptible to breast cancer metastasis.
There is growing awareness that part of that susceptibility is due to host factors. The host factors are the characteristics of the non-malignant cells and the general biological environment surrounding the malignant breast tumor.
Sometimes the host factors are referred to as the pre-metastatic niche and it is thought that bone-marrow-derived progenitor cells may directly influence the dissemination of malignant cells to distant areas.
Non-neoplastichost cells within the tumor may also play a key role in the regulation of breast cancer metastasis.