A Hormone Receptor Status Is Either Hormone Receptor Positive Or Hormone Receptor Negative
- Hormone receptor-positive breast cancer cells have either estrogen or progesterone receptors. These breast cancers can be treated with hormone therapy drugs that lower estrogen levels or block estrogen receptors. HR-positive cancers tend to grow more slowly than those that are HR-negative. HR-positive cancers are generally more common in women after menopause.
- Hormone receptor-negative breast cancers do not have estrogen or progesterone receptors. These types of cancers will not benefit from hormone therapy drugs and typically grow faster than HR-positive cancers. HR-negative cancers are more common in women who have not yet gone through menopause.
How Is Hormone Therapy Used
Your doctor will consider the hormone status of your breast cancer when they plan your treatment. One of the main treatments for PR-positive breast cancer is hormone therapy, which keeps HR-positive cancer cells from using hormones to grow.
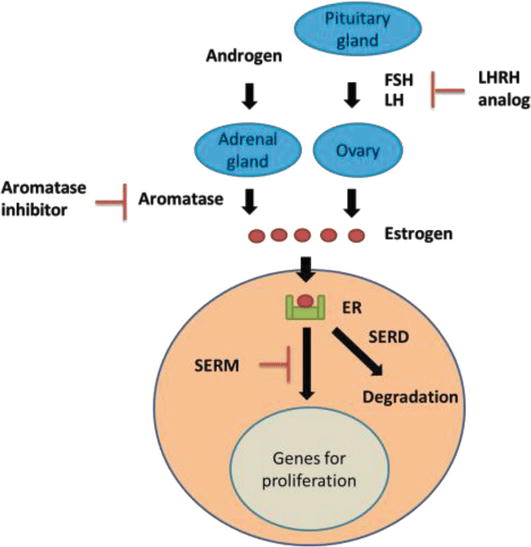
- Hormone therapy works by removing hormones from your body or blocking their ability to attach to the receptors on your cells. There are two main ways you may get hormone therapy:
- Surgery to take out your ovaries so your body doesnât make any more breast-cancer-related hormones
Hormone therapy pills or shots, which keep your body from making female hormones or block the receptors so hormones canât attach to cancer cells
The type you get will depend in part on whether youâve gone through menopause yet.
Hormone therapy can be part of treatment for any stage of HR-positive breast cancer. You may get it along with other treatments, such as surgery or chemotherapy, depending on the stage of your cancer.
If your cancer can be removed with surgery, is early stage , or is limited to the place it first started in your breast , you might get hormone therapy:
- Before surgery to help shrink the tumor
- After surgery, with or without chemotherapy, to decrease the chance that the cancer will come back
If you have inflammatory breast cancer or the tumor has spread from where it first started , you might get hormone therapy after surgery.
Hormone Receptors & Receptor Tests
All breast cancers are examined under a microscope for biomarkers of estrogen and progesterone receptors. About 70% of breast cancers are hormone receptor-positive.
Your hormone receptor status should appear on your pathology report after biopsy or surgery. Receptors will be retested if you ever have a recurrence or metastases as well, as your status can change.
Hormones and receptors go together kind of like a lock and key. Receptors are proteins on the surface of breast cells, and when hormones bind to them, the receptors tell the cells to grow and divide. All breast cells have receptors, but they are found in much greater numbers on breast cancer cells that are considered positive.
A goal of treatment is to block the signal created when the hormones attach to receptors. Doing that requires one of two things:
Most of the time, breast cancers tend to be positive or negative for both estrogen and progesterone receptors. Now and then, one will be positive for estrogen but not progesterone. The treatment is the same either way.
You May Like: What Hormones Affect Hair Loss
Read Also: What Does Inflammatory Breast Cancer Look Like
What Are Hormones And Hormone Receptors
Hormones are substances that function as chemical messengers in the body. They affect the actions of cells and tissues at various locations in the body, often reaching their targets through the bloodstream.
The hormones estrogen and progesterone are produced by the ovaries in premenopausal women and by some other tissues, including fat and skin, in both premenopausal and postmenopausal women and in men. Estrogen promotes the development and maintenance of female sex characteristics and the growth of long bones. Progesterone plays a role in the menstrual cycle and pregnancy.
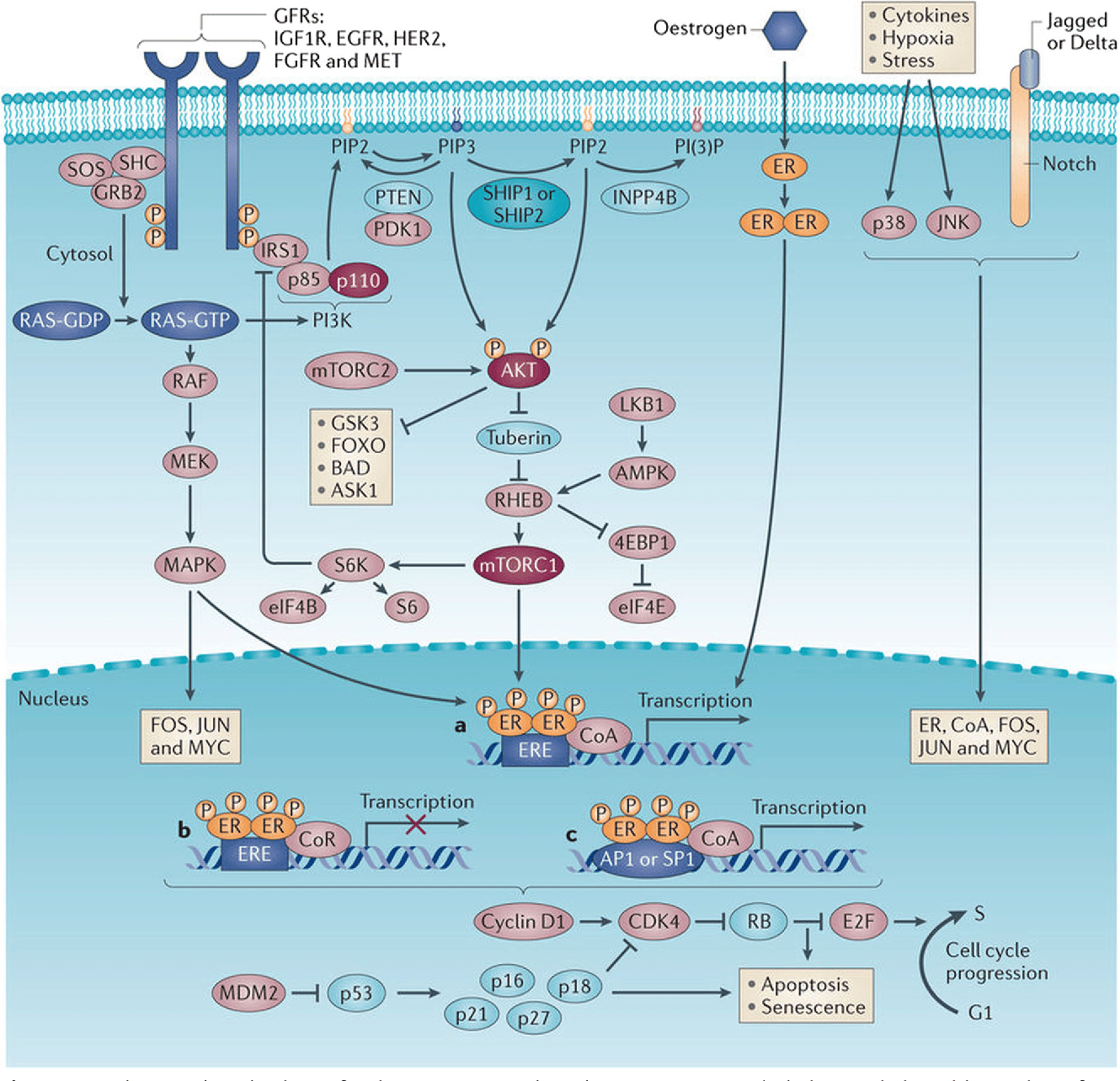
Estrogen and progesterone also promote the growth of some breast cancers, which are called hormone-sensitive breast cancers. Hormone-sensitive breast cancer cells contain proteins called hormone receptors that become activated when hormones bind to them. The activated receptors cause changes in the expression of specific genes, which can stimulate cell growth.
Breast cancers that lack ERs are called ER negative, and if they lack both ER and PR they may be called HR negative.
Approximately 67%80% of breast cancers in women are ER positive . Approximately 90% of breast cancers in men are ER positive and approximately 80% are PR positive .
What Is The Primary Source Of Estrogen In The Body
After menopause, fat is the primary source of estrogen production in the body. This means that weight is a critical factor in determining estrogen levels, for both pre and post-menopausal women. Dietary choices and activities that promote a healthy weight are essential to any estrogen-reducing program.
Recommended Reading: What Are The Two Types Of Breast Cancer
How Is Hormone Therapy Used To Treat Breast Cancer
There are three main ways that hormone therapy is used to treat hormone-sensitive breast cancer:
Adjuvant therapy for early-stage breast cancer:Tamoxifen is FDA approved for adjuvant hormone treatment of premenopausal and postmenopausal women with ER-positive early-stage breast cancer, and the aromatase inhibitorsanastrozole, letrozole, and exemestane are approved for this use in postmenopausal women.
Research has shown that women who receive at least 5 years of adjuvant therapy with tamoxifen after having surgery for early-stage ER-positive breast cancer have reduced risks of breast cancer recurrence, including a new breast cancer in the other breast, and reduced risk of death at 15 years .
Until recently, most women who received adjuvant hormone therapy to reduce the chance of a breast cancer recurrence took tamoxifen every day for 5 years. However, with the introduction of newer hormone therapies , some of which have been compared with tamoxifen in clinical trials, additional approaches to hormone therapy have become common .
Some premenopausal women with early-stage ER-positive breast cancer may have ovarian suppression plus an aromatase inhibitor, which was found to have higher rates of freedom from recurrence than ovarian suppression plus tamoxifen or tamoxifen alone .
Men with early-stage ER-positive breast cancer who receive adjuvant therapy are usually treated first with tamoxifen. Those treated with an aromatase inhibitor usually also take a GnRH agonist.
Icb Monotherapy In Hr+ Breast Cancer
In the phase 1b JAVELIN trial, 168 heavily pretreated patients with metastatic breast cancer, regardless of subtype or PD-L1 status, were treated with the PD-L1 inhibitor, avelumab . Of the 168 patients, 72 had HR+/HER2- disease and the ORR for this group was 2.8% compared to 5.2% in the TNBC group. The median duration of response was not reached. In addition, subgroup analysis by PD-L1 status did not reveal any trend in efficacy. Given the low ORR, avelumab was determined to have limited therapeutic benefit as monotherapy in patients with metastatic HR+/HER2- breast cancer. Altogether, the KEYNOTE-028 and JAVELIN trials revealed the limited single-agent efficacy of ICB in HR+ breast cancer, particularly in heavily pretreated disease. The limited response to ICB monotherapy led to the inclusion of chemotherapy and other systemic therapeutics that may have synergism with ICB, a strategy used in TNBC.
Recommended Reading: Metaplastic Breast Cancer Survival Rate
Factors To Consider When Discussing Adjuvant Systemic Therapy
Clinical decision-making is a complex process that incorporates patient and tumor characteristics, the expected benefit of systemic therapy, individualized prognostic information and patient preference. Several large groups have provided guidance for the use of adjuvant systemic therapy in early stage HR-positive breast cancer. Cancer Care Ontario and ASCO guidelines recommend consideration of patient demographics such as age, menopausal status and co-morbidities when making adjuvant
Clinicopathologic Characteristics Of Single Hormone Receptor
The median follow-up duration for the 6,980 patients included in this analysis was 45 months . In this study, 4,651 cases were double HR+ tumors, 1,758 were double HR- tumors, and 571 cases were single hormone-receptor positive tumors, of which 90 cases were ER-PR+ tumors and 481 were ER + PR- tumors. The clinicopathological characteristics of the four subtypes are summarized in Table . Overall, ER+/PR- tumors were found more frequently in postmenopausal women than other subtypes . Compared with ER + PR+ tumor, ER + PR- tumors were not significantly different in staging , but ER+PR- tumors exhibited higher nuclear grade , higher Ki-67 level , and higher EGFR and HER2 expression . However, compared with ER-PR- tumors, ER + PR- tumors showed lower stage , lower NG , lower Ki-67 level , lower p53 expression and lower EGFR expression , but there was no difference in HER2 overexpression .
Table 1 Clinicopathologic characteristics of patients with ER + PR+, ER + PR-, ER-PR+ and ER-PR- tumors
ER-PR+ tumors had higher NG , higher Ki-67 level , and higher expression of p53 and EGFR than ER + PR+ tumors. However, compared with ER-PR- tumors, there was no difference in stage or NG . Also, there was no difference in expression of Ki-67 , p53 , EGFR or HER2 .
Don’t Miss: Do 18 Year Olds Get Breast Cancer
Her2 Status In Breast Cancer
If your cancer appears to be aggressive and fast-growing, you might have higher levels of a protein called human epidermal growth factor receptor 2, or HER2 for short. Some genes, like HER2, and the proteins they make, do more than play a role in the development of breast cancer. They can also influence how your breast cancer behaves as well as how it may respond to specific cancer treatments.
Usually, HER2 receptors help control how a healthy breast cell grows, divides, and repairs itself. However, if the HER2 gene doesnt work correctly and produces too many copies of itself, it leads to the uncontrolled growth of breast cancer cells.
If You Cant Have Surgery
Surgery is the main treatment for breast cancer, but some women have health problems that mean they cant have surgery. Some women choose not to have surgery.
In this case, if your breast cancer is oestrogen receptor positive, your doctor might recommend hormone therapy. This treatment wonât get rid of the cancer but can stop it growing or shrink it.
The treatment can often control the cancer for some time. Your doctor might change you to a different type of hormone treatment if your cancer starts growing again.
You May Like: How Common Is Inflammatory Breast Cancer
If Cancer Comes Back Or Has Spread
AIs, tamoxifen, and fulvestrant can be used to treat more advanced hormone-positive breast cancers, especially in post-menopausal women. They are often continued for as long as they are helpful. Pre-menopausal women might be offered tamoxifen alone or an AI in combination with an LHRH agonist for advanced disease.
Treatment Tailoring In Hormone
RT-PCR, reverse transcriptase-PCR. Modified from Sotiriou & Pusztai .
One of such tools, the Oncotype DX, merits to be addressed in more details . This test was developed to answer the following question Is it possible to identify a woman with hormone receptor-positive, lymph node-negative breast cancer, for whom it may be necessary something more than just tamoxifen alone? Among the 16 genes that the Oncotype DX analyzes, some are related to the ER , other related to cell proliferation , and other, like HER2, which are not functionally related. The relative expression of these genes compared with that of five reference genes whose expression does not correlate with tumor aggressiveness is combined by a mathematical formula that results in a continuous score ) that is directly proportional to the risk of metastatic relapse. The RS has been into divided into three risk categories by cutoffs that were established studying the clinical outcome of women enrolled in the tamoxifen arm of the NSABP B-20 clinical trial . The low-risk group has been defined by a RS< 18, the intermediate by a RS between 18 and 30, and the high risk by a RS> 30.
| 28 | 32 |
RS, recurrence score NSABP, national surgical adjuvant breast and bowel project ECOG, eastern cooperative oncology group SWOG, south western oncology group.
Don’t Miss: Who Is The Best Doctor For Breast Cancer
Can Other Drugs Interfere With Hormone Therapy
Certain drugs, including several commonly prescribed antidepressants , inhibit an enzyme called CYP2D6. This enzyme plays a critical role in the body’s use of tamoxifen because CYP2D6 metabolizes, or breaks down, tamoxifen into molecules, or metabolites, that are much more active than tamoxifen itself.
The possibility that SSRIs might, by inhibiting CYP2D6, slow the metabolism of tamoxifen and reduce its effectiveness is a concern given that as many as one-fourth of breast cancer patients experience clinical depression and may be treated with SSRIs. In addition, SSRIs are sometimes used to treat hot flashes caused by hormone therapy.
Many experts suggest that patients who are taking antidepressants along with tamoxifen should discuss treatment options with their doctors, such as switching from an SSRI that is a potent inhibitor of CYP2D6, such as paroxetine hydrochloride , to one that is a weaker inhibitor, such as sertraline or citalopram , or to an antidepressant that does not inhibit CYP2D6, such as venlafaxine . Or doctors may suggest that their postmenopausal patients take an aromatase inhibitor instead of tamoxifen.
Other medications that inhibit CYP2D6 include the following:
- quinidine, which is used to treat abnormal heart rhythms
What Hormones Are Responsible For Cancer Growth
When the hormones estrogen and progesterone attach to these receptors, they fuel the cancer growth. Cancers are called hormone receptor-positive or hormone receptor-negative based on whether or not they have these receptors . Knowing the hormone receptor status is important in deciding treatment options.
You May Like: Free Stuff For Breast Cancer Patients 2021
Selective Estrogen Receptor Response Modulators
Selective estrogen receptor response modulators attach to and block estrogen receptors in breast cells. This stops the estrogen from signaling to the cells to grow.
Examples of SERMs include:
- toremifene for people with advanced ER-positive breast cancer after menopause
A doctor may prescribe one of these drugs with another medication.
Side effects
Possible adverse effects of SERMs include:
- changes in mood
- vaginal dryness or unusual discharge
Less commonly, SERMs may increase the risk of:
from the age of 5074. Those aged 4049 years should ask their doctor about whether screening is a good idea.
Other organizations have different recommendations. For example, the ACS recommends annual breast screenings for females aged 4554 years .
However, each persons situation is different. A doctor may recommend a different screening schedule for someone with a higher risk of breast cancer.
The outlook for people with ER-positive breast cancer tends to be good, especially when a doctor diagnoses it early.
A person with an early diagnosis of any type of breast cancer has a 99% chance of living for at least another 5 years, and often longer, the ACS reports.
However, if the cancer has spread to other organs, the chance of surviving for at least another 5 years is 29%, it notes.
Taking these steps may ultimately lead to a better outlook if a person develops breast cancer:
Less Common Types Of Hormone Therapy
Some other types of hormone therapy that were used more often in the past, but are rarely given now include:
- Megestrol acetate , a progesterone-like drug
- Androgens , like testosterone
These might be options if other forms of hormone therapy are no longer working, but they can often cause side effects.
Don’t Miss: What Medications Are Used For Breast Cancer
What Are The Symptoms
Many women donât have any symptoms of breast cancer when they get a diagnosis. Instead, doctors find it during a routine mammogram screening.
HR-positive breast cancer has the same symptoms as other types of breast cancer. Some of the more common symptoms include:
- A new lump in your breast
- Swelling of part or all of your breast
- Pain in your breast or nipple
- Changes in the skin over your breast
- Swollen lymph nodes, which may feel like lumps under your arm or near your collarbone
What Happens If You Have Her2
Excess of HER2 results in overgrowth of the abnormal breast cells, giving rise to HER2-positive cancer. When you have been diagnosed with breast cancer, doctors check if you have HER2-positive or HER2-negative breast cancer. The type of breast cancer is diagnosed based on tests that check for the presence of HER2 protein in the breast tissue.
Read Also: What To Say To Someone With Breast Cancer
Rna Extraction And Qpcr
Total RNA was extracted using TRIzol® reagent and miRNeasy kits according to the manufacturer’s protocol. The miRNA was converted to cDNA by using the PrimeScript® RT reagent kit according to the manufacturer’s protocol. MiR-206, TGF- mRNAs, and genes of the TGF- signaling pathway family were analyzed by qPCR in triplicate using 100 ng cDNA and SYBR® Premix Ex Taq on an Applied Biosystems 7500 Fast Real-Time PCR System . The miRNA and mRNA fold changes were determined using the CT method with normalization to U6 snRNA and GAPDH, respectively. The primers are listed in Supplementary Methods .
Side Effects Of Tamoxifen And Toremifene

The most common side effects of tamoxifen and toremifene are:
- Vaginal dryness or discharge
- Changes in the menstrual cycle
When tamoxifen treatment starts, a small number of women with cancer that has spread to the bones might have a tumor flare which can cause bone pain. This usually decreases quickly, but in some rare cases a woman may also develop a high calcium level in the blood that is hard to control. If this happens, the treatment may need to be stopped for a time.
Rare, but more serious side effects are also possible:
Don’t Miss: Can Triple Negative Breast Cancer Be Hereditary