What Nutrients Do Cancer Cells Need To Grow
To maintain their ability to grow at a breakneck pace, cancer cells consume nutrients at an increased rate. Glutamine, which is the most abundant amino acid in plasma is one of them. Some types of cancer become heavily reliant on this versatile molecule as it offers energy, carbon, nitrogen, and antioxidant properties, all of which support tumor growth and survival, Dias said.
Systemic Therapy For Metastatic Disease
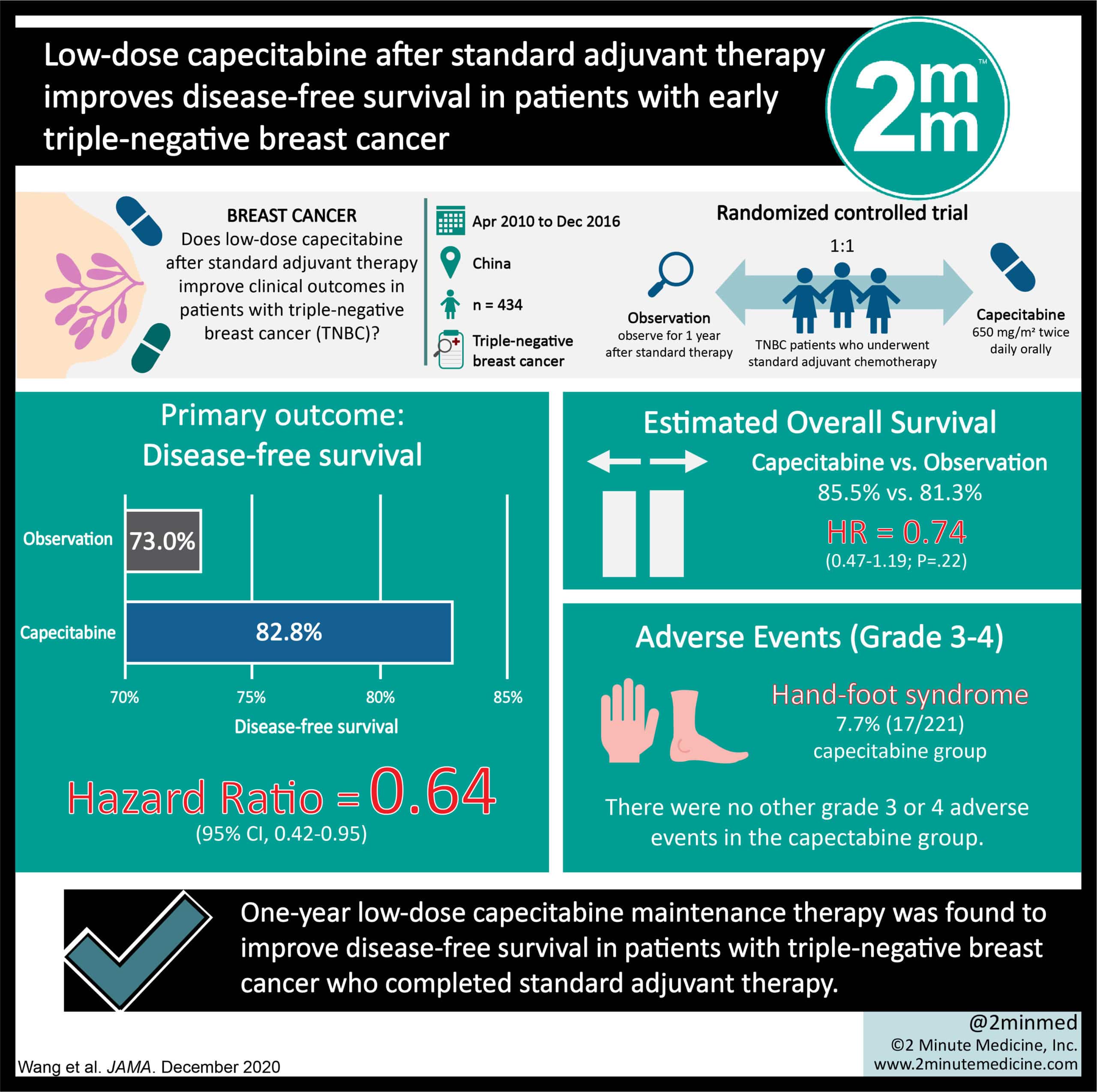
Patients with metastatic TNBC experience poorer outcomes when compared with patients with other breast cancer subtypes51. First-line systemic treatment typically includes a taxane or anthracycline combination55, and median OS tends to be 18 months or less5658. Novel treatment approaches are critical to improve these dire survival outcomes.
Targeted Drug Therapy For Breast Cancer
Targeted drug therapy uses medicines that are directed at proteins on breast cancer cells that help them grow, spread, and live longer. Targeted drugs work to destroy cancer cells or slow down their growth. They have side effects different from chemotherapy and can be given in the vein , as an injection under the skin, or as a pill.
Some targeted therapy drugs, for example, monoclonal antibodies, work in more than one way to control cancer cells and may also be considered immunotherapy because they boost the immune system.
Like chemotherapy, these drugs enter the bloodstream and reach almost all areas of the body, which makes them useful against cancers that have spread to distant parts of the body. Targeted drugs sometimes work even when chemo drugs do not. Some targeted drugs can help other types of treatment work better.
Several types of targeted therapy drugs can be used to treat breast cancer.
Dont Miss: Breast Cancer Stage 3
Read Also: Signs And Symptoms Of Metastatic Breast Cancer
Editorial Note On The Review Process
F1000 Faculty Reviews are commissioned from members of the prestigiousF1000 Faculty and are edited as a service to readers. In order to make these reviews as comprehensive and accessible as possible, the referees provide input before publication and only the final, revised version is published. The referees who approved the final version are listed with their names and affiliations but without their reports on earlier versions .
The referees who approved this article are:
- Heather L. McArthur, Cedars-Sinai Medical Center, Los Angeles, CA, USACompeting interests: Heather McArthur has previously consulted or had an advisory role for Merck, Spectrum Pharmaceuticals, Lilly, Amgen, Immunomedics, Pfizer, Genentech, Bristol-Meyers Squibb and Genomic Health.Additionally, Heather was on the expert panel for Lilly in 2017.
- Kazuaki Takabe, Division of Breast Surgery, Department of Surgical Oncology, Roswell Park Cancer Institute, Buffalo, NY, USA Department of Surgery, Jacobs School of Medicine and Biomedical Sciences, The State University of New York Buffalo, Buffalo, NY, USANo competing interests were disclosed.
Androgen Receptor Targeted Agents
Hormone receptor negative BC generally does not respond to endocrine-targeted therapies. In a previous study done at Memorial Sloan-Kettering Cancer Center, a subset of estrogen/progesterone receptor -negative cancers were identified and shown to have a transcriptional profile like the molecular apocrine or luminal androgen receptor AR . Accordingly, the hypothesis that AR inhibition would potentially benefit patients with AR +ve ER/PgR negative advanced BC was tested using different therapies and the results are listed below.
5.4.1. Bicalutamide
Bicalutamide is a non-steroidal AR antagonist approved by the FDA in combination with luteinizing hormone-releasing hormone in the treatment of metastatic prostate cancer . A multicenter phase II trial was conducted to evaluate the efficacy Bicalutamide in ER/PgR negative metastatic BC. Patients enrolled in the study were administered 150 mg of Bicalutamide orally every day and they were treated until disease progression or intolerable side effects were observed . The patient population enrolled in this trial represents TNBC. Furthermore, in the subset of patients with AR +ve ER/PgR negative metastatic BC, a clinical benefit rate of 19% was noted, realizing this studys endpoint . This treatment was well-tolerated, and the adverse events reported included fatigue, hot flashes, limb edema, and transaminase elevation . This study supports the hypothesis that targeting AR could benefit patients with ER/PgR negative metastatic BC.
Recommended Reading: Surgery To Remove Breast Cancer
What You Need To Know
- Triple-negative breast cancer accounts for about 10% to 20% of all breast cancer cases.
- Every cancer diagnosis is unique, but in general, triple-negative breast cancer is a more aggressive type of tumor with a faster growth rate, higher risk of metastasis and recurrence risk. Therefore, it often requires chemotherapy as part of the treatment.
- Surgery is also an important part of treatment, but if a tumor is small and localized, mastectomy may not be necessary. Chemotherapy can shrink triple-negative breast tumors, and patients can become candidates for less-extensive surgery.
- Triple-negative cancers are more common in patients with hereditary genetic mutations, and genetic counseling and testing should be considered.
Search Results And General Characteristics Of Included Literature
According to the search strategy, a total of 784 studies were screened out. After reading the full text according to the protocol, 28 studies including seven treatment methods were included in this study. The literature screening process is shown in Figure 1. The basic characteristics and results of the included studies are shown in Table 2.
|
Table 2 Main Characteristics and Results of the Eligible Studies |
|
Figure 1 Flow chart of literature screening included in this study. |
Also Check: Diet For Breast Cancer Patients
Triple Negative Breast Cancer Recurrence
Triple negative breast cancer has a high rate of recurrence or return within the first three years after treatment, but then theres a marked reduction after five years. Some factors may increase ones risk of recurrence, such as being diagnosed at age 35 or younger, having a large tumor or cancer cells in the lymph nodes at the time of diagnosis or undergoing a lumpectomy without radiation therapy.
New Treatments Bring Hope For Those With Triple
Sign up for our newsletters to get GMA delivered to your inbox every morning!
For years, triple-negative breast cancer has been perceived as aggressive with little hope of treatment, but that thought appears to be changing among experts as more promising treatment options develop.
“I would say that the future is bright for triple-negative breast cancer,” said Dr. Erica Mayer, a medical oncologist and senior physician at Dana-Farber Cancer Institute in Boston. “We now have new treatment strategies that we didn’t have available before that definitely seem to be benefiting patients with triple-negative disease.”
Triple-negative breast cancer is the smallest category of breast cancer groups, only accounting for about 10-15% of all breast cancers, according to the American Cancer Society. Mayer says this doesn’t mean that it’s uncommon. “Because breast cancer is a very common cancer, there are actually tens of thousands of people who are diagnosed with triple-negative breast cancer every year.”
While lacking those receptors, triple-negative breast cancer still has the same symptoms as other types. Some of these symptoms are a new lump or mass in the breast or armpit, dimpling of the breast skin, abnormal nipple discharge or even the nipple turning inward.
- Actress opens up about fighting stage 3 breast cancer at age 19 October 5, 2021
Don’t Miss: Early Stage Breast Cancer Treatment
What To Drink And Eat
Matcha Tea: Every morning is just better when it starts with tea, or really any time of day for that matter! Once you know that this type of tea contains epigallocatechin-3-gallate , which can kill cancer cells by limiting angiogenesis, prevent DNA damage, and may stop the production of breast cancer stem cellsit is even more of a treat! Matcha tea provides up to 137 times more EGCG than regular green tea! So drink upI suggest 2 cups a day of this type of Matcha Tea. It is also packed with antioxidants, vitamin C, tocopherols, carotenoids, selenium, zinc, chromium, and manganese. Matcha also detoxifies heavy metals and toxic chemicals while burning fat and boosting your metabolism.
Drinking tea is also a great life metaphor. We are like teawe dont know our strength until we are in hot water -says many revolutionary women. Right now, you are realizing just how strong you are and then finding even more power, my dear conqueror. Buy Matcha Tea.
Blueberries: A berry delicious way to increase the number of cancer destroying Natural Killer cells in the body and slow or stop the growth of Breast Cancer Stem Cells is to enjoy a handful of organic blueberries every day. This study found that these berries can cause apoptosis in TNBC cells! You can also order a blueberry concentrate from Life Extension if you are trying to keep your sugars down. Here is my full report on these little superheroes, and I highly suggest this delectable Blueberry Chia Pudding!
An Immunotherapy For Tnbc
Immunotherapy represents a different approach. Instead of going after cancer cells directly, immunotherapy drugs work by stimulating the patients own immune system to fight the cancer.
PD-L1 inhibitors, also called checkpoint inhibitors, work by releasing the brakes on the immune system.
As I wrote in a post late last year, in 2019 the FDA approved the first checkpoint inhibitor for use in breast cancer treatment. The drug approved last year is Tecentriq , and is given in combination with chemotherapy, for patients with metastatic TNBC and tumors expressing the biomarker, PD-L1.
In November 2020, the FDA granted accelerated approval for a second checkpoint inhibitor, Keytruda , also to be given in combination with chemotherapy, for patients with metastatic TNBC whose tumors express the marker PD-L1.
Keytruda has already been approved for a number of different types of cancer, but not for breast cancer.
Also Check: What Is The Breast Cancer Gene Called
Immune Checkpoint Blockade With Monotherapy
As noted on clinicaltrials.gov , approximately half of the registered studies are focused on immune checkpoint blocking-related therapies. Of these, greater than 100 clinical studies have already entered phase II or phase III, implying that immunotherapy is an important trend in TNBC treatment. Previous trials have shown positive results with pembrolizumab or atezolizumab monotherapy in TNBC. In the KEYNOTE-012 trial , 27 PD-L1-positive TNBC patients exhibited an ORR of 18.5%, and the median time to response was 17.9 weeks . Another targeting PD-L1 mAb, atezolizumab, was also reported to be safe and clinically active in mTNBC. In this phase I study , the evaluation of PD-L1 expression levels demonstrated an improved ORR, a longer OS, and a higher disease control rate in patients with at least 1% TILs expressing PD-L1. Interestingly, patients receiving first-line atezolizumab therapy exhibited a better prognosis , suggesting the superiority of atezolizumab combined with first-line.
Different Drugs Same Target
Breast cancers that are HER2-positive tend to be aggressive, with the excess HER2 protein on tumor cells fueling the cancers growth. In the late 1990s, trastuzumab was among the first targeted cancer therapies to be approved by FDA, after trials showed it could improve survival in women with metastatic HER2-positive breast cancer.
Over time, other HER2-targeted therapies emerged, some with alternative mechanisms for disrupting HER2 activity in cancer cells. Drugs like trastuzumab and pertuzumab are monoclonal antibodies that bind to the HER2 protein above the cancer cells surface, preventing it from acting or enlisting the immune system to help destroy cells that produce it.
Tucatinib, on the other hand, is a member of a class of drugs known as tyrosine kinase inhibitors . These drugs work by binding to the part of the HER2 protein that is inside the cell and preventing it from sending signals that promote cell growth. Other HER2-targeted TKIs include neratinib and lapatinib .
Some TKIs have multiple targets. But, compared with other HER2-targeted drugs, tucatinib appears to be relatively selective for HER2that is, its less likely to bind to related proteins, explained Stanley Lipkowitz, M.D., Ph.D., chief of the Womens Malignancies Branch in NCIs Center for Cancer Research. That selectivity limits the risk of side effects seen with other HER2-targeted TKIs that inhibit other targets, Dr. Lipkowitz said.
Don’t Miss: What Is Chemotherapy For Breast Cancer
What Is The Stage Of Triple Negative Breast Cancer
Stages I-III triple-negative breast cancer. If the early-stage TNBC tumor is small enough to be removed by surgery, then breast-conserving surgery or a mastectomy with a check of the lymph nodes may be done. In certain cases, such as with a large tumor or if the lymph nodes are found to have cancer, radiation may follow surgery.
What About Hdc And Asct
One of the largest and best controlled clinical trials evaluating the use of high-dose chemotherapy and autologous stem cell transplant to treat patients with early stage breast cancer and more than 9 involved axillary lymph nodes continues to show survival benefit 20 years from receiving treatment. In fact HDC was associated with improved overall survival in the subgroup of women with triple-negative breast cancers: 52.9% of these patients were alive at 20 years compared with 37.5% of those in the conventional-dose chemotherapy.11
In the 1990s HDC and ASCT was increasingly used to treat breast cancer and other solid tumors based on its success in curing certain individuals with lymphoma, leukemia, and multiple myeloma. HDC continue to be the standard of care for many cancers but became out of favor as a treatment option for breast cancer due to conflicting study results and concerns about side effects.
The use of HDC for the treatment of breast cancer was based on the idea that breast cancer treatment could be improved if higher doses of chemotherapy could be administered and this has been borne out to be true. A standard treatment for high risk early stage breast cancer today is dose-dense chemotherapy which is widely used instead of HDC and ASCT and requires the use of blood cell growth boosters to ensure the chemotherapy can be safely administered in a timely manner.
You May Like: Is Stage 4 Metastatic Breast Cancer Curable
Combinations Of Immune Checkpoint Inhibitors
However, most patients with TNBC do not respond well to PD-1 or PD-L1 monotherapy therefore, inducing a favorable tumor immune microenvironment appears to be particularly important. Conventional chemotherapeutic agents, such as taxane, cisplatin, and cyclophosphamide, can enhance tumor antigen release, improve the tumor microenvironment, and add the possibility of an antitumor response . Biopsies before and after NAC showed that the immune microenvironment was altered from low TIL to high TIL, and patients with high TIL levels exhibited improved survival . For example, paclitaxel has pleiotropic immune-modulating effects because it helps mature dendritic cells shift the T-helper phenotype to promote the secretion of proinflammatory cytokines and enhance the activity of CD8+ T cells . An animal model has shown evidence that cisplatin markedly induces tumor regression and improves survival when combined with anti-PD-1 and anti-cytotoxic lymphocyte antigen 4 . These studies suggest that ICB combined with chemotherapy may achieve a synergistic or additive clinical effect.
In addition to the combination of PARPi and immunotherapy, a series of trials of immunotherapy in combination with other drugs have entered clinical studies . For example, alternative PD-1/PD-L1 ICB combined with tyrosinase inhibitors has entered phase III studies .
Table 4 Unpublished phase III trials of immunotherapy for TNBC
Chemotherapy For Triple Negative Breast Cancer
TNBC has historically had limited treatment options when compared to other types of BC. The mainstay of treatment for TNBC remains cytotoxic chemotherapy, despite the emergence of new biologic and targeted agents. The therapeutic benefits of cytotoxic chemotherapy in TNBC are well established, with comprehensive data on the efficacy of chemotherapy in the neoadjuvant, adjuvant, and metastatic settings. Compared with hormone receptor-positive BC, the use of chemotherapy regimens in the neoadjuvant treatment of TNBC has a significantly higher pathological response rate and can considerably ameliorate the prognosis of TNBC patients . Nevertheless, TNBC carries an overall inferior prognosis despite its chemo-sensitivity . The use of neoadjuvant systemic treatment in the early stages is becoming the standard of care in TNBCs and is associated with higher pathological complete response rates as compared to other BC subtypes . Patients who achieve pCR with primary therapy have improved survival outcomes . As such, pCR is predictive of improved long-term outcomes for TNBC and is a reliable endpoint in clinical trials evaluating the efficacy of neoadjuvant chemotherapy.
Don’t Miss: How Do They Do Chemo For Breast Cancer
Update On Metastatic Triple Negative Breast Cancer Treatment
Triple-negative breast cancer is a breast cancer subtype that tests negative for estrogen receptors , progesterone receptors , and human epidermal growth factor receptors 2 . Since TNBC tumors lack known targets for drug development, the treatment options have been mostly limited to chemotherapy.
Recently, however, new treatment options have become available, including immunotherapy, PARP inhibitors and the antibody drug conjugate Trodelvy . Additionally, there are other types of drugs and regimens currently being studied in clinical trials, including drugs targeting the PI3K/AKT/mTOR pathway, the androgen receptor pathway, and regimens that combine PARP inhibitors, immune checkpoint inhibitors and other types of drugs.
See below for information on current treatment options and drugs currently being studied in clinical trials.
Overview of Approved and Investigational Drugs for TNBC
Role Of Poly Polymerase Inhibitors And Chemotherapy Forbrca1 Andbrca2 Mutation Carriers
The OlympiAD clinical trial randomly assigned patients with advanced HER2-negative breast cancer and a germlineBRCA mutation to a PARP inhibitor, olaparib , or standard physicians choice chemotherapy59. The significant progression-free survival benefit favoured olaparib with a median PFS of 7.2 months 59. Subgroup analysis of PFS for randomised stratification factors revealed an outstanding HR for progression of 0.39 amongst the TNBC subset, which made up nearly 50% of the treatment cohorts in both arms59.
The EMBRACA clinical trial compared the PARP inhibitor talazoparib with protocol-specified standard therapy and found a favourable median PFS of 8.6 versus 5.6 months in the standard therapy group with a trend towards an OS benefit, but the data are immature60. Although rates of adverse events were similar in the two treatment arms, patients randomly assigned to talazoparib reported superior quality-of-life outcomes with a significant delay in the onset of a clinically meaningful deterioration in global health status60.
The results of the randomised phase 3 trials BRAVO using niraparib 300 mg daily61 versus chemotherapy and BROCADE using veliparib or placebo combined with chemotherapy in a similar cohort are still pending.
Don’t Miss: How Many People Get Breast Cancer